# Navigating the Diabetes Spectrum: Understanding Type 1, Type 2, and Gestational Diabetes with Insights from the American Diabetes Association
Diabetes is one of the most prevalent chronic conditions affecting millions of people worldwide. Understanding the differences between the types of diabetes—Type 1, Type 2, and Gestational Diabetes—is vital for effective management and prevention. The American Diabetes Association (ADA) provides comprehensive insights that help navigate the complexities of this condition. In this article, we will explore the nuances of each diabetes type and how to manage them effectively, ensuring a well-rounded understanding for patients and caregivers alike.
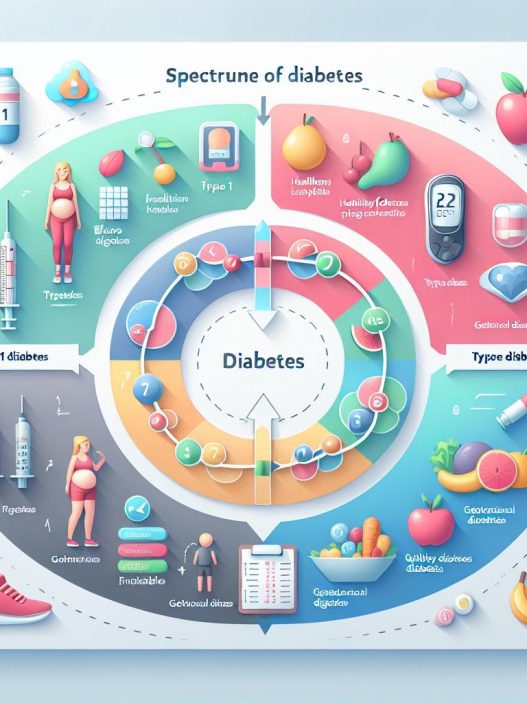
Types of Diabetes: An Overview of Type 1, Type 2, and Gestational Diabetes
Diabetes can be broadly classified into three primary types: Type 1, Type 2, and Gestational Diabetes. Each type has its unique causes, symptoms, and treatment options, and understanding these differences is essential for effective management.
Type 1 Diabetes is an autoimmune condition that typically manifests in childhood or early adulthood. In this form of diabetes, the immune system mistakenly attacks insulin-producing beta cells in the pancreas, resulting in little or no insulin production. This lack of insulin means that glucose cannot enter cells effectively, leading to elevated blood sugar levels. Individuals with Type 1 Diabetes require lifelong insulin therapy to manage their blood glucose levels and prevent complications.
In contrast, Type 2 Diabetes is often linked to lifestyle factors and tends to develop in adulthood, although it is increasingly being diagnosed in children and adolescents. This form of diabetes occurs when the body becomes resistant to insulin or when the pancreas does not produce enough insulin to maintain normal glucose levels. Type 2 Diabetes is often associated with obesity, physical inactivity, and poor dietary choices. Management typically involves lifestyle changes, monitoring blood sugar, and in some cases, medication.
Gestational Diabetes occurs during pregnancy and usually resolves after childbirth. However, it poses significant risks for both the mother and the baby, including increased chances of developing Type 2 Diabetes later in life. Hormonal changes during pregnancy can lead to insulin resistance, resulting in elevated blood sugar levels. Management of Gestational Diabetes involves monitoring blood sugar levels, dietary adjustments, and physical activity to ensure the health and wellbeing of both mother and child.
The Importance of Early Diagnosis and Management of Diabetes
Early diagnosis of diabetes is crucial for effective management and prevention of long-term complications. In many cases, individuals may remain asymptomatic in the early stages of the disease, making routine screenings essential, especially for those at risk. According to the American Diabetes Association, risk factors for Type 2 Diabetes include a family history of the disease, obesity, high blood pressure, and sedentary lifestyle.
Identifying diabetes early allows for appropriate interventions, including lifestyle modifications, regular monitoring of blood sugar levels, and possible medication. For Type 1 Diabetes, early recognition of symptoms such as excessive thirst, frequent urination, extreme fatigue, and unexplained weight loss can be a lifesaver. Education on how to recognize and respond to these symptoms is vital for individuals and their families.
Moreover, delayed diagnosis can lead to severe complications, such as cardiovascular disease, kidney damage, vision loss, and neuropathy. The ADA emphasizes the need for routine health check-ups and awareness campaigns to educate the public about the risks associated with diabetes. Implementing preventive measures can significantly reduce the likelihood of developing diabetes and improve overall health outcomes.
Managing Type 1 Diabetes: Insulin Therapy and Lifestyle Adjustments
Type 1 Diabetes management primarily revolves around insulin therapy, which involves a delicate balancing act of insulin doses and carbohydrate intake. Unlike those with Type 2 Diabetes who may manage their condition through lifestyle changes and oral medications, individuals with Type 1 Diabetes depend on insulin injections or infusions. Modern delivery methods include insulin pens, insulin pumps, and continuous glucose monitors (CGMs) that provide real-time feedback on blood sugar levels.
Education plays a critical role in managing Type 1 Diabetes. Patients must learn to administer insulin correctly, check their blood sugar levels, and understand the relationship between food, exercise, and insulin needs. The ADA encourages comprehensive diabetes education that covers these aspects and also highlights the importance of emotional support and mental health in managing chronic conditions.
Lifestyle adjustments can also enhance the effectiveness of diabetes management. Regular physical activity, a balanced diet rich in whole grains, lean proteins, and healthy fats are crucial for maintaining stable blood sugar levels. It’s important to tailor these adjustments to meet individual preferences and lifestyle needs, promoting both adherence to the regimen and overall well-being.
Strategies for Managing Type 2 Diabetes: Lifestyle and Medication
Type 2 Diabetes management typically begins with lifestyle modifications aimed at achieving a healthy weight and improving insulin sensitivity. The foundation of this approach includes a balanced diet rich in vegetables, fruits, whole grains, and lean proteins while reducing the intake of added sugars and processed foods. Meal planning can help individuals make healthier choices and keep blood sugar levels stable.
In addition to dietary changes, regular physical activity is a key component of managing Type 2 Diabetes. The ADA recommends engaging in at least 150 minutes of moderate aerobic exercise per week, along with strength training exercises twice a week. Physical activity not only improves insulin sensitivity but also aids in weight management, reducing the risk of complications.
When lifestyle changes alone are not enough to control blood sugar levels, healthcare providers may prescribe oral medications or insulin therapy. There are various classes of medications available, each with different mechanisms of action. It’s vital for individuals to work closely with their healthcare team to determine the most effective treatment plan tailored to their needs.
Understanding Gestational Diabetes: Risks and Management
Gestational Diabetes is a temporary condition occurring during pregnancy but requires careful management to protect the health of both mother and baby. Women at higher risk for developing Gestational Diabetes include those who are overweight, older than 25, or have a family history of diabetes. Early screening, typically conducted around the 24th to 28th week of pregnancy, is crucial for timely diagnosis and intervention.
Management of Gestational Diabetes focuses on diet and physical activity to keep blood sugar levels within a target range. Working with a healthcare team, including a dietitian, can help expectant mothers create a personalized meal plan that meets their nutritional needs while avoiding spikes in blood sugar. Regular physical activity is also encouraged, as it can help improve insulin sensitivity and contribute to overall well-being.
Monitoring blood glucose levels becomes essential during this time, with frequent check-ups to assess progress. While many women can manage Gestational Diabetes through lifestyle changes alone, some may need insulin or medication to maintain blood sugar control. Following delivery, blood sugar levels should return to normal; however, women who have had Gestational Diabetes are at a higher risk for developing Type 2 Diabetes later in life.
Long-term Health Implications of Diabetes and the Role of the American Diabetes Association
The long-term implications of diabetes can be severe, impacting various bodily systems and significantly reducing quality of life. Persistent high blood sugar levels can lead to complications that affect cardiovascular health, renal function, eye health, and nerve integrity. The ADA emphasizes that achieving and maintaining optimal blood sugar levels is essential for preventing these complications.
Regular check-ups and screenings for potential complications are integral to diabetes management. This includes routine eye exams, foot care assessments, and kidney function tests. The ADA provides guidelines and resources for individuals to understand when to seek medical intervention and how to partner effectively with healthcare providers to monitor and manage their conditions.
Moreover, public awareness and education are crucial in fighting the diabetes epidemic. The American Diabetes Association engages in numerous advocacy efforts to educate communities, partner with healthcare professionals, and promote research aimed at finding better treatments and, ultimately, a cure for diabetes. Their initiatives also include support programs for individuals and families affected by diabetes, providing them with tools and resources necessary for effective management.
By spreading knowledge and breaking down misconceptions about diabetes, the ADA plays a vital role in shaping public health policy and encouraging healthy practices that can mitigate the diabetes epidemic’s impact.
—
In conclusion, navigating the diabetes spectrum—understanding Type 1, Type 2, and Gestational Diabetes—requires informed decision-making and proactive management. Thanks to resources like the American Diabetes Association, individuals can equip themselves with the knowledge necessary to lead healthier lives and mitigate the risks associated with this chronic condition. By taking a comprehensive approach to diabetes education, management strategies, and lifestyle modifications, we can work toward reducing the prevalence and impact of diabetes in our communities.