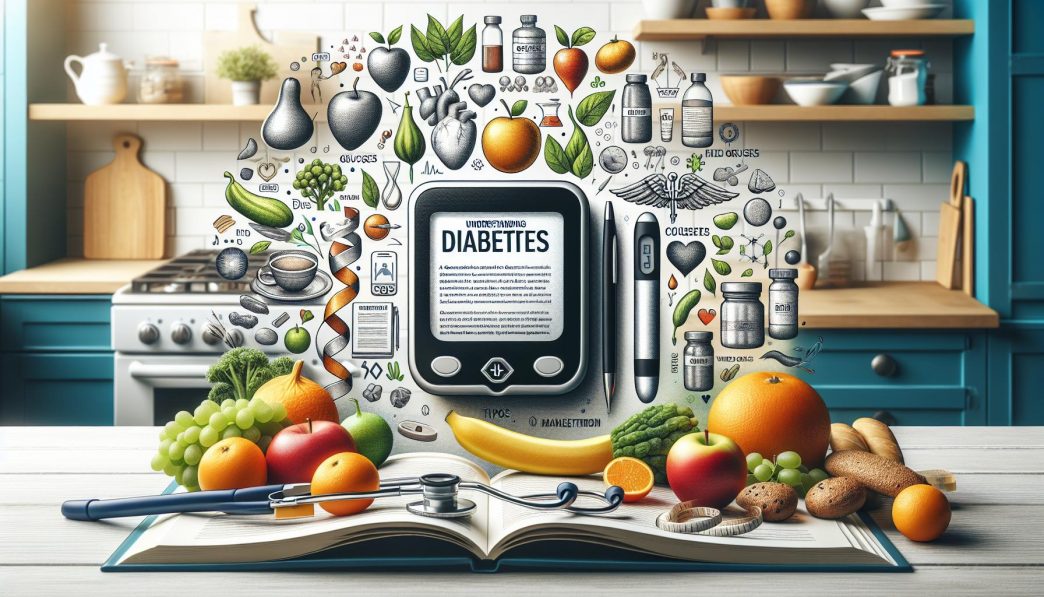
# Understanding Diabetes: A Comprehensive Guide to Types, Causes, and Management
Diabetes is a chronic health condition that affects millions of people worldwide, influencing how the body processes glucose and can potentially lead to serious health issues if not managed properly. This comprehensive guide explores the various types of diabetes, their causes, symptoms, and effective management strategies to help those living with this condition lead healthier lives.
What is Diabetes? An Overview of the Condition
Diabetes is characterized by high blood sugar levels over an extended period. This elevated blood sugar is primarily due to inadequate insulin production, insulin resistance, or both. Insulin is a hormone produced by the pancreas that facilitates glucose entry into cells for energy. When the body cannot utilize insulin effectively, it results in various metabolic complications, leading to long-term health risks such as cardiovascular disease, kidney failure, and vision problems.
The World Health Organization (WHO) has classified diabetes into several types, each with distinct causes and characteristics. Understanding the different forms of diabetes is crucial for effective diagnosis, treatment, and management strategies. With lifestyle changes, medications, and regular monitoring, individuals can successfully manage their diabetes and maintain a good quality of life.
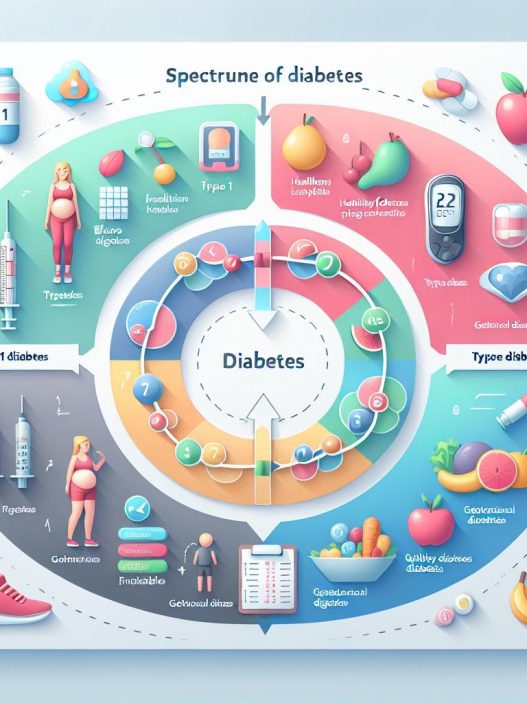
The Different Types of Diabetes: Distinguishing Between Them
Diabetes is generally classified into three main categories: Type 1, Type 2, and gestational diabetes. Each type has unique attributes and challenges associated with it.
Type 1 Diabetes
Type 1 diabetes is an autoimmune condition wherein the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This form of diabetes commonly develops in children and young adults, although it can occur at any age. Individuals with Type 1 diabetes require continuous insulin administration to manage blood glucose levels since their bodies cannot produce insulin.
Diagnosis typically occurs in childhood or adolescence. Symptoms often include increased thirst, frequent urination, fatigue, and unexplained weight loss. Immediate treatment is essential to prevent diabetic ketoacidosis, a life-threatening condition that occurs when the body breaks down fat for energy instead of glucose.
Type 2 Diabetes
Type 2 diabetes is characterized by insulin resistance, where the body’s cells do not respond effectively to insulin. This form of diabetes predominantly affects adults, although it is increasingly being diagnosed in younger individuals due to the rise of obesity and sedentary lifestyles. Over time, the pancreas may also fail to produce enough insulin to maintain normal blood sugar levels.
Common risk factors for Type 2 diabetes include obesity, age, family history, and physical inactivity. Symptoms can be subtle and may include increased hunger, fatigue, and blurred vision. Unlike Type 1, individuals with Type 2 diabetes may manage their condition with lifestyle modifications, oral medications, or insulin therapy as needed.
Gestational Diabetes
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased demands. This condition typically resolves after childbirth, but it can increase the risk of developing Type 2 diabetes later in life for both the mother and the child. Gestational diabetes can cause complications for both mothers and babies, including high birth weight and preterm delivery.
Women at higher risk of developing gestational diabetes include those with a family history of diabetes, older age, and excessive weight before pregnancy. Regular screening during pregnancy is essential to identify and manage this condition effectively.
Causes of Diabetes: Unpacking the Risk Factors
Understanding the myriad of causes that lead to diabetes is vital for prevention and management. Numerous risk factors, including genetics, environment, lifestyle choices, and body weight, interplay to contribute to the onset of diabetes.
Genetic Factors
Genetics plays a significant role in determining an individual’s risk of developing diabetes. Family history is a crucial factor; if a person has a parent or sibling with diabetes, their risk increases significantly. Specific genes associated with insulin production and glucose metabolism have been identified, indicating a hereditary component to Type 1 and Type 2 diabetes.
While genetic predisposition cannot be altered, awareness of family history can aid in early detection and proactive lifestyle adjustments to decrease risk.
Obesity and Sedentary Lifestyle
Obesity is one of the most significant risk factors for developing Type 2 diabetes. Excess body fat, particularly visceral fat around the abdomen, contributes to insulin resistance, making it more difficult for the body to regulate blood sugar levels. Sedentary lifestyles further increase this risk, as regular physical activity helps to maintain optimal weight, reduces stress, and improves insulin sensitivity.
It is vital for individuals at risk to engage in regular physical activity and maintain a healthy weight through a balanced diet rich in whole grains, fruits, vegetables, lean protein, and healthy fats.
Age and Hormonal Changes
As individuals age, their risk of developing diabetes increases, primarily due to the natural decline in insulin production and increased insulin resistance. Hormonal changes associated with aging also affect glucose metabolism and body composition.
Moreover, specific life stages, such as pregnancy, introduce hormonal fluctuations that can influence blood sugar levels, exemplified by gestational diabetes. Regular monitoring of blood sugar levels becomes essential as one ages, whether one has an existing diagnosis or is simply at risk.
Symptoms of Diabetes: Recognizing the Signs
Early detection of diabetes can prevent severe complications and improve management outcomes. Individuals must be aware of common symptoms and seek medical advice if they suspect diabetes.
Common Symptoms
Typical symptoms of diabetes can vary depending on the type but often include increased thirst, frequent urination, extreme fatigue, and blurry vision. Individuals may also experience slow-healing wounds, tingling in the hands and feet, and unexplained weight loss. These symptoms develop gradually, particularly in Type 2 diabetes, which may remain unnoticed for years.
Being vigilant about minor changes in health can facilitate early diagnosis and successful management plans. Regular health check-ups and blood glucose evaluations are crucial for those at risk.
Complications of Untreated Diabetes
If left untreated, diabetes can lead to serious long-term complications, including cardiovascular disease, kidney damage, nerve damage, and eye problems. Diabetic retinopathy, for example, is a severe eye condition that can lead to blindness. Similarly, peripheral neuropathy can cause disabling nerve pain and loss of sensation.
Preventative actions and timely medical interventions can significantly mitigate these risks. Regular consultations with healthcare professionals, including endocrinologists and dietitians, can pave the way for better health trajectories.
Management Strategies: How to Control Diabetes Effectively
Managing diabetes involves a multi-faceted approach that focuses on blood sugar control, lifestyle modifications, medication adherence, and regular monitoring.
Dietary Management
Nutrition plays a critical role in diabetes management. Individuals with diabetes should prioritize a well-balanced diet that emphasizes whole foods and minimizes processed sugars and unhealthy fats. Carbohydrate counting can help in understanding the impact of food on blood sugar levels.
Incorporating fiber-rich foods such as whole grains, legumes, fruits, and vegetables can improve glucose regulation. Furthermore, engaging in mindful eating practices, such as portion control and regular meal times, can help stabilize blood sugar levels throughout the day.
Physical Activity
Regular physical activity not only aids in weight management but also enhances insulin sensitivity, allowing cells to use glucose more effectively. The American Diabetes Association recommends at least 150 minutes of moderate aerobic activity each week alongside strength training exercises on two or more days of the week.
Engaging in activities such as walking, swimming, or cycling can provide immense health benefits. Moreover, finding enjoyable activities will encourage consistent participation in exercise regimens.
Medication and Insulin Therapy
Depending on the type and severity of diabetes, medication or insulin therapy may be necessary. Type 1 diabetes typically requires daily insulin injections, while Type 2 diabetes may be managed through oral medications that enhance insulin sensitivity or stimulate insulin production.
Regular consultations with healthcare professionals are essential to ensure that the management plan remains effective and appropriate. Adjustments may be necessary depending on ever-changing health conditions, lifestyle factors, and individual responses to treatment.
The Role of Mental Health in Diabetes Management
Diabetes management goes beyond physical health; mental wellness is equally crucial. Living with a chronic condition can lead to emotional challenges, including anxiety and depression, which can further complicate diabetes management.
Emotional Impact of Diabetes
The emotional burden of managing diabetes can sometimes lead to “diabetes burnout,” where individuals feel overwhelmed and disconnected from their management plans. It is essential for those living with diabetes to identify and address these feelings, as they can lead to poor self-care practices and unhealthy coping mechanisms.
Support from healthcare professionals, family, and peer groups can foster a sense of community and accountability, which aids in maintaining motivation and engagement in diabetes management.
Mindfulness and Stress Management Strategies
Practicing mindfulness and stress-reduction techniques can significantly improve overall health outcomes for people with diabetes. Techniques such as meditation, yoga, and deep-breathing exercises can facilitate relaxation and help individuals cope with the stresses of daily life and diabetes management.
Additionally, maintaining a healthy work-life balance and carving out time for self-care can help individuals manage their mental health, thus positively impacting their diabetes management journey.
The Future of Diabetes Management: Innovations and Outlook
The landscape of diabetes management is evolving with advancements in technology, research, and treatment options.
Technological Advancements in Monitoring
Continuous glucose monitors (CGMs) provide real-time blood glucose data, allowing for more precise management of diabetes. These devices can alert users to abnormal blood sugar levels, enabling timely interventions. Smartphone apps for tracking diet, exercise, and medication adherence can empower individuals to take control of their diabetes management.
Moreover, the advent of insulin pumps and automated insulin delivery systems showcases the technological strides that are improving the lives of individuals with diabetes.
Research and Innovations in Treatment
Research into diabetes is ongoing, with several promising treatments on the horizon. Innovations such as artificial pancreas systems, which automatically adjust insulin delivery based on real-time glucose levels, present the potential for enhanced diabetes management.
Additionally, studies on regenerative medicine and immunotherapy could pave the way for breakthroughs in Type 1 diabetes treatment, potentially reversing the autoimmune conditions leading to insulin deficiency.
Community Support and Health Initiatives
The importance of community support cannot be overstated in managing diabetes effectively. Local health initiatives focusing on education, access to resources, and support networks can foster a sense of belonging and empowerment.
Many organizations provide valuable resources, including workshops, support groups, and educational materials, promoting awareness and understanding of diabetes management. Collaborations between healthcare providers, community organizations, and affected individuals can create a robust support system for better health outcomes.
—
This comprehensive guide has navigated through the complexities of diabetes, covering its types, causes, symptoms, management strategies, mental health considerations, and future innovations. Understanding diabetes is crucial for those directly affected and their loved ones, transforming engagement and empowering individuals to lead healthier lives. Adopting proactive measures and staying informed can significantly impact the course of diabetes management, leading to a brighter and healthier future.