[ad_1]
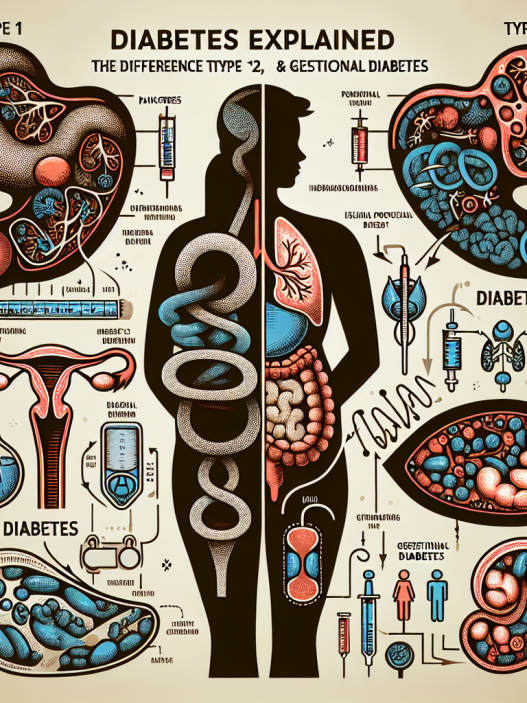
Diabetes is a complex and chronic condition affecting millions worldwide. Understanding its nuances is crucial for managing not only the disease but also its long-term implications on overall health. Insights gleaned from the American Diabetes Association’s National Conference are invaluable for healthcare professionals, patients, and caregivers alike. In this extensive blog post, we will explore key takeaways, emerging research, and expert opinions that stem from this pivotal event, aiming to shed light on the multifaceted nature of diabetes.
Recent Advances in Diabetes Research
The American Diabetes Association’s National Conference serves as a beacon for the latest advancements in diabetes research. Scientists and healthcare professionals worldwide gather to share groundbreaking studies focusing on diabetes prevention, management, and potential cures. Recent findings highlight the importance of personalized medicine in diabetes care, suggesting that treatments should be tailored to individual patient profiles rather than a one-size-fits-all approach. Emerging technologies, such as continuous glucose monitoring systems, have revolutionized how diabetes is managed day-to-day, providing real-time data that empowers patients to make informed decisions about their health.
Additionally, there has been significant progress in understanding the genetic factors that contribute to type 1 and type 2 diabetes. Researchers presented case studies illustrating how specific genetic markers can predict an individual’s risk of developing diabetes. This knowledge paves the way for proactive measures to be implemented, such as lifestyle changes or early intervention strategies tailored to those identified as high-risk. Attendees learned about the importance of incorporating genetic counseling into diabetes care, offering a holistic approach that embraces both biology and lifestyle.
Nutrition and Its Impact on Diabetes Management
Diet plays a critical role in the management of diabetes, and the National Conference brought to light several key dietary strategies that can significantly influence blood glucose levels. One session focused on the glycemic index (GI) and its relevance in daily meal planning. Foods with a low GI are digested more slowly, leading to gradual increases in blood sugar levels. Healthcare providers emphasized the importance of educating patients about the benefits of choosing low-GI foods, such as whole grains, legumes, and non-starchy vegetables.
A significant discussion also revolved around the Mediterranean diet and its advantages for individuals with diabetes. Studies showcased at the conference showed that adherence to this dietary pattern can improve glycemic control, decrease cardiovascular risk, and enhance overall health outcomes. The diet’s emphasis on healthy fats, lean proteins, and abundant fruits and vegetables aligns well with diabetes management goals, providing the necessary nutrients without excessive caloric intake. Conference speakers encouraged participants to intertwine cultural food preferences with these dietary recommendations, creating personalized meal plans that are both enjoyable and beneficial.
Another emerging trend in diabetes nutrition highlighted at the conference was the role of plant-based diets. Numerous studies showcased the positive effects of vegetarian and vegan diets on insulin sensitivity and weight management. Speakers advocated for integrating more plant-based foods into patients’ diets, along with educating them on how to maintain balance and nutritional adequacy while adopting these lifestyles. They stressed that fostering a supportive community around meal planning can further encourage sustainable dietary changes.
Technological Innovations in Diabetes Care
Technology is transforming diabetes care, and the National Conference presented an array of innovative solutions that are shaping the future of diabetes management. One of the notable advancements discussed was the evolution of insulin delivery systems. Smart insulin pens and automated insulin delivery systems are now being developed to improve the precision of insulin dosing. These devices utilize algorithms and data from continuous glucose monitors (CGMs) to automatically adjust insulin delivery, thereby reducing the risk of hypoglycemia and improving overall glycemic control.
Moreover, the conference highlighted developments in digital health applications designed to support diabetes management. Mobile apps that integrate with CGMs allow users to visualize trends and patterns in their blood sugar levels, log their food intake, and receive personalized recommendations. Speakers noted the potential of these technologies to enhance patient engagement and facilitate better communication between healthcare providers and patients. The data collected can also be used in research to better understand how lifestyle factors impact diabetes management.
Another exciting technological innovation discussed was the use of artificial intelligence (AI) in diabetes care. AI can analyze vast amounts of data to identify patterns and correlations that may not be evident through traditional analysis. This capability can lead to the development of predictive models to forecast blood sugar fluctuations and suggest interventions preemptively. Conference experts encouraged healthcare professionals to embrace these technologies to provide personalized care while ensuring patients remain informed and empowered in their management.
Psychosocial Factors in Diabetes Management
Understanding diabetes requires more than just focusing on physical health; psychosocial factors play a significant role in diabetes management as well. A notable theme at this year’s National Conference was the importance of mental health in managing chronic diseases like diabetes. Experts discussed the high prevalence of anxiety and depression among diabetic patients and how these mental health issues can adversely affect glycemic control and overall health outcomes.
Presenters emphasized the necessity for healthcare providers to screen patients for psychosocial issues routinely. Building a supportive healthcare environment that recognizes and addresses emotional well-being can lead to improved self-management and adherence to treatment plans. Strategies discussed included integrating mental health professionals into diabetes care teams and using cognitive-behavioral therapies to help patients cope with the emotional burden of diabetes.
Additionally, self-care was a significant topic, highlighting the need for strategies that promote emotional resilience and self-management skills. Conference attendees learned about the importance of supportive peer networks in empowering diabetic patients. The emotional support from others with similar experiences can foster a sense of community, reducing feelings of isolation that often accompany chronic illness. Utilizing group sessions or online platforms can help patients connect, share their stories, and encourage one another in their journeys toward better health.
Policy and Advocacy Efforts in Diabetes Care
The American Diabetes Association is at the forefront of policy advocacy aimed at improving diabetes care and access to resources. During the National Conference, attendees learned about ongoing initiatives to promote legislative changes that enhance healthcare access for individuals with diabetes. Presenters discussed the impact of healthcare disparities on marginalized communities, emphasizing the need for targeted policies that address these gaps.
Policy advocates shared success stories from grassroots campaigns that led to positive legislative changes, such as improved funding for diabetes education and access to diabetes supplies. The conversation highlighted the necessity of collaboration among healthcare professionals, patients, and policymakers to create an environment that supports diabetes management. Education and advocacy are critical components of driving awareness surrounding the needs of people living with diabetes at various socioeconomic levels.
Moreover, conference discussions focused on the importance of health insurance coverage for diabetes technologies, such as CGMs and insulin pumps. Attendees were urged to advocate for policies ensuring that these crucial tools are both accessible and affordable for all patients. As diabetes care continues to evolve, ongoing advocacy is essential for ensuring that patients receive the best possible support for their health journey.
In summary, the American Diabetes Association’s National Conference provides a wealth of knowledge and insights into various aspects of diabetes management. By delving into recent research advancements, nutrition, technological innovations, psychosocial factors, and policy advocacy, we gain a comprehensive understanding of diabetes and its complexities. Each element contributes to the overarching goal of improving health outcomes and enhancing the quality of life for individuals living with diabetes. As we continue to broaden our understanding, informed strategies can evolve, empowering patients and improving care in ways that were once unimaginable.
[ad_2]