# Understanding the Spectrum of Diabetes: A Comprehensive Guide to Type 1, Type 2, and Gestational Diabetes
Diabetes is a multifaceted condition that affects millions globally, manifesting in various forms such as Type 1, Type 2, and Gestational Diabetes. Understanding these types can enhance awareness, promote earlier diagnosis, and foster proper management strategies. This extensive guide delves into the spectrum of diabetes, offering insightful information about its causes, symptoms, and treatments to help you navigate this complex landscape effectively.
Understanding Diabetes: An Overview
Diabetes is a chronic metabolic disorder characterized by high blood sugar levels due to the body’s inability to produce enough insulin or utilize it effectively. This condition can have far-reaching consequences if not properly managed. Statistically, diabetes affects over 400 million people worldwide, highlighting the necessity for a deeper understanding of its complexities.
There are three primary types of diabetes to consider: Type 1, Type 2, and Gestational Diabetes. Each type arises from different mechanisms within the body and necessitates unique approaches in treatment and management. In this section, we will explore the fundamental characteristics of these diabetes types, emphasizing their distinct etiologies and presentations.
The Distinct Features of Type 1 Diabetes
Type 1 Diabetes (T1D) is an autoimmune condition where the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This leads to absolute insulin deficiency, requiring individuals with T1D to rely on external insulin sources for survival. T1D usually manifests in childhood or adolescence but can occur at any age.
Symptoms of Type 1 Diabetes often develop rapidly, with common indicators including excessive thirst, frequent urination, extreme hunger, fatigue, and blurred vision. If left untreated, it can cause severe complications such as diabetic ketoacidosis (DKA), a life-threatening condition. Early diagnosis and insulin therapy are critical for managing Type 1 Diabetes effectively and preventing complications.
Heredity plays a significant role in the development of Type 1 Diabetes. Genetic predisposition, combined with environmental factors, is believed to play a crucial role in the onset of this disease. Although there is no known way to prevent Type 1 Diabetes, ongoing research endeavors aim to uncover potential avenues for prevention and treatment, fostering hope for those affected.
The Complexities of Type 2 Diabetes
Type 2 Diabetes (T2D) is the most prevalent form of diabetes, accounting for more than 90% of all diabetes cases. It typically arises from insulin resistance, where the body’s cells no longer respond effectively to insulin secretion. Over time, the pancreas cannot produce enough insulin to maintain normal glucose levels, leading to chronic hyperglycemia.
Unlike Type 1, Type 2 Diabetes can often be managed and even reversed with lifestyle modifications, including a healthy diet, regular exercise, and weight management. However, many individuals may remain asymptomatic for years, only to discover their condition through routine blood testing. Common symptoms include increased thirst, frequent urination, fatigue, and blurred vision, similar to those seen in Type 1 Diabetes.
Various risk factors contribute to the development of Type 2 Diabetes, including obesity, sedentary lifestyle, family history, and age. As our lifestyles and eating habits have evolved, so too has the prevalence of T2D, making awareness and prevention strategies crucial. Education around proper nutrition, physical activity, and regular monitoring of blood glucose levels is pivotal in combating this condition in communities worldwide.
Gestational Diabetes: Unique Challenges During Pregnancy
Gestational Diabetes (GD) occurs when a woman, during pregnancy, develops insulin resistance leading to elevated blood sugar levels. This condition typically arises in the second or third trimester and affects approximately 2-10% of pregnant women, posing various risks to both mother and baby if not effectively managed.
Women who develop Gestational Diabetes may experience similar symptoms to those seen in both Type 1 and Type 2 Diabetes; however, many may remain asymptomatic. Therefore, routine screening during pregnancy is critical, usually conducted around the 24th to 28th week of gestation, to identify and manage this condition promptly.
The management of Gestational Diabetes primarily involves dietary modifications, glucose monitoring, and, if necessary, insulin therapy. Successfully controlling blood sugar levels during pregnancy is paramount, as uncontrolled GD can lead to consequences such as macrosomia (excessive birth weight), and the potential for Type 2 Diabetes later in life for both mother and child. Postpartum follow-up is essential to ensure the proper health of both the mother and child and to manage ongoing insulin sensitivity.
Common Symptoms Across All Types of Diabetes
While the presentation of diabetes can vary significantly between its types, certain symptoms are commonly shared. Frequent urination, persistent thirst, extreme hunger, fatigue, and blurred vision are warning signs that demand attention. Recognizing these symptoms early can lead to prompt diagnosis and intervention, crucial for effective management and improving quality of life.
For instance, the frequent urination associated with elevated blood sugar levels occurs because the kidneys attempt to flush out excess glucose through urine. This results in dehydration, prompting increased thirst. Similarly, the demands placed on the body can lead to fatigue, as cells lack the glucose necessary for energy production. Thus, awareness of these symptoms is vital.
Understanding these shared symptoms can help individuals distinguish between normal variations and indicators of a potential diabetes diagnosis. Regular check-ups and screenings are essential for detecting diabetes early despite the absence of overt symptoms, especially for high-risk individuals.
Complications Related to Diabetes: Long-Term Risks
Complications of diabetes can be severe and wide-ranging, affecting nearly every organ system in the body. Short-term complications include conditions such as Ketoacidosis and Hyperglycemic Hyperosmolar State (HHS), while long-term complications may manifest as cardiovascular disease, neuropathy, nephropathy, and retinopathy, among others.
Cardiovascular disease is a significant risk for individuals with diabetes, as hyperglycemia can damage blood vessels and nerves that control the heart. Studies have shown that people with diabetes are at a higher risk for heart attacks and strokes, emphasizing the importance of effective management strategies to control blood sugar levels and maintain cardiovascular health.
Additionally, neuropathy, a condition characterized by nerve damage, particularly in the extremities, can lead to symptoms such as tingling, numbness, or pain. In severe cases, it can result in infections, ulcers, and even amputations. Regular foot care and monitoring can help mitigate the risk of complications associated with neuropathy.
Managing Diabetes: A Holistic Approach
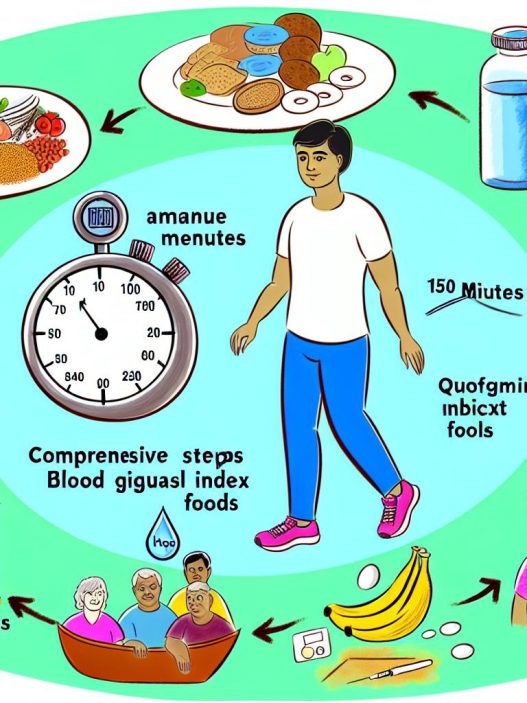
Effective diabetes management requires a multifaceted approach that integrates medical treatment, lifestyle modifications, and self-management education. Blood sugar monitoring is vital to understand patterns, adjust treatment plans, and proactively manage the condition.
Nutritional education plays a crucial role in effective management, focusing on balanced diets rich in nutrients while being mindful of carbohydrate intake. Monitoring the glycemic index of foods can also aid in maintaining stable blood sugar levels. Consulting with a registered dietitian specializing in diabetes can provide personalized meal plans that suit individual needs and preferences.
In addition to nutrition, physical activity is essential in managing diabetes. Regular exercise enhances insulin sensitivity, aids in weight management, and improves overall well-being. Healthcare professionals often recommend a mix of aerobic and strength training exercises tailored to individual capabilities and preferences, ensuring sustainable physical activity habits.
By integrating medical, nutritional, and exercise management, individuals with diabetes can significantly enhance their quality of life while minimizing complications. Education and consistent healthcare follow-up are pivotal in fostering a proactive management approach, allowing individuals to take charge of their health.
### Conclusion
Understanding the spectrum of diabetes—Type 1, Type 2, and Gestational Diabetes—is crucial for promoting awareness and fostering effective management strategies. By recognizing the signs and symptoms associated with each type, individuals can seek timely medical guidance, leading to better control of their condition. Through education, lifestyle modifications, and holistic approaches, the challenges posed by diabetes can be addressed effectively, paving the way for a healthier and more fulfilled life.
This comprehensive guide serves as a foundation for ongoing discussions around diabetes, encouraging individuals to remain empowered in their health journeys while promoting broader awareness in their communities. The increasing incidence of diabetes underlines the urgency for a collective response, prioritizing education, prevention, and management strategies at both individual and societal levels.