# Understanding the Spectrum of Diabetes: From Type 1 to Type 2 and Beyond
Diabetes is a chronic disease that affects millions worldwide, disrupting the body’s ability to regulate blood sugar. Understanding the spectrum of diabetes—including Type 1, Type 2, and other forms like gestational and LADA—is crucial for effective management and prevention. This comprehensive guide will delve into the various types of diabetes, their symptoms, diagnoses, treatments, and current research, offering invaluable insights for patients, caregivers, and healthcare professionals alike.
Understanding the Different Types of Diabetes
Diabetes is not a one-size-fits-all condition. The two most prevalent forms—Type 1 and Type 2 diabetes—represent different etiologies and management strategies. Type 1 diabetes is an autoimmune disorder where the immune system attacks insulin-producing beta cells in the pancreas, resulting in little to no insulin production. Those diagnosed with Type 1 usually present in childhood or adolescence, but it can occur at any age.
On the other hand, Type 2 diabetes is characterized by insulin resistance and is primarily associated with lifestyle factors, including obesity, inactivity, and genetics. Unlike Type 1, Type 2 diabetes can often be managed or even reversed through lifestyle modifications such as diet and exercise. Together, these two types account for the vast majority of diabetes cases, but they are just the tip of the iceberg when exploring this complex condition.
Symptoms and Diagnosis of Diabetes
Recognizing the symptoms of diabetes is essential for early detection and treatment. Common symptoms include excessive thirst, frequent urination, increased hunger, fatigue, blurred vision, and slow-healing sores. However, the symptoms can vary widely from one individual to another, sometimes leading to misdiagnosis or under-diagnosis. For instance, many people with Type 2 diabetes may be asymptomatic for years before they are diagnosed, highlighting the need for routine screenings, especially for high-risk groups.
Diagnosis typically involves blood tests that measure blood glucose levels. The most common tests include the fasting plasma glucose test, the oral glucose tolerance test, and the A1C test, which provides an average blood glucose level over the past two to three months. Healthcare providers often consider a combination of symptoms and lab results to make an accurate diagnosis, emphasizing the importance of recognizing early signs and symptoms.
Managing Type 1 Diabetes
Management of Type 1 diabetes requires a comprehensive approach that combines regular insulin therapy with careful monitoring of blood glucose levels. Patients often use insulin pumps or multiple daily injections to provide the necessary insulin to control their blood sugar levels effectively. Additionally, understanding carbohydrate counting and its impact on blood sugar is vital. Patients must learn to balance their insulin dosage with food intake and physical activity.
Education plays a significant role in the management of Type 1 diabetes. Continuous education helps patients understand how different foods, stress levels, and exercise impact blood glucose control. Regular check-ups with healthcare providers, including endocrinologists and dietitians, are essential in adjusting treatment plans based on lifestyle changes and individual responses to insulin.
Moreover, emerging technologies, such as continuous glucose monitors (CGMs) and artificial pancreas systems, are enhancing the management of Type 1 diabetes. These tools provide real-time feedback, allowing for more precise adjustments and better overall glycemic control. Patients equipped with these technologies can enjoy a better quality of life while managing a complex and often unpredictable condition.
Managing Type 2 Diabetes
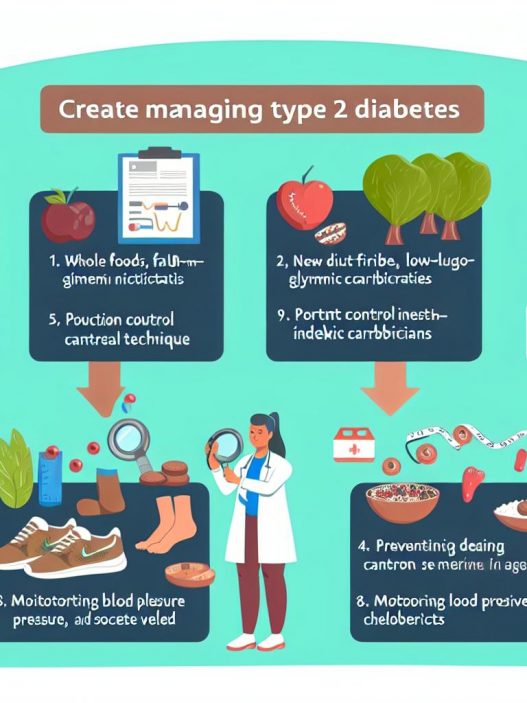
Managing Type 2 diabetes often begins with lifestyle modifications aimed at improving insulin sensitivity. Nutritional therapies focus on balanced diets rich in whole grains, lean proteins, healthy fats, and ample fruits and vegetables. Weight loss, even a modest one, can have significant effects on controlling blood sugar levels and reducing the need for medication.
In addition to dietary changes, exercise plays a crucial role in managing Type 2 diabetes. Regular physical activity improves insulin sensitivity, lowers blood sugar levels, and can lead to weight loss. A combination of aerobic activities, like walking or cycling, and strength training is generally encouraged to reap the maximum health benefits. Providers often recommend setting achievable fitness goals to keep patients motivated and engaged.
When lifestyle changes are insufficient, oral medications or insulin therapy may be necessary. Various classes of medications are available, each working through different mechanisms to manage blood sugar. Understanding the options and working closely with healthcare providers can help patients find the most effective treatment plan tailored to their individual needs.
Understanding Gestational Diabetes
Gestational diabetes is a temporary form of diabetes that occurs during pregnancy when the body cannot produce enough insulin to meet increased demands. Although generally resolved following delivery, it poses risks for both the mother and the baby, including higher chances of developing Type 2 diabetes later in life.
Pregnant individuals should undergo screening for gestational diabetes around the 24th to 28th week of pregnancy. Common symptoms are often subtle or non-existent, making screenings essential. If diagnosed, management typically involves dietary changes, physical activity, and, in some cases, insulin therapy to maintain appropriate blood sugar levels and ensure a healthy pregnancy outcome.
Education about the condition is crucial for expecting mothers, who must learn to monitor their blood sugar levels and make lifestyle adjustments that benefit both themselves and their babies. Postpartum monitoring is equally important, as women with gestational diabetes are at a higher risk for developing Type 2 diabetes in the following years.
Exploring Other Forms of Diabetes
While Type 1 and Type 2 diabetes are the most commonly discussed, several other forms exist that merit attention. Latent Autoimmune Diabetes in Adults (LADA) is often misclassified as Type 2 diabetes, as it presents similarly but has an autoimmune component similar to Type 1 diabetes. Understanding LADA is essential for proper treatment; misdiagnosis can lead to ineffective interventions.
Additionally, Monogenic diabetes, caused by genetic mutations, and secondary diabetes, which can develop due to other health conditions such as pancreatitis, are increasingly recognized in diabetes care. Awareness of these forms can contribute to more precise diagnoses and tailored treatment options.
Research is ongoing to differentiate these lesser-known diabetes forms from Type 1 and Type 2. As our understanding evolves, tailored treatments and management strategies will likely improve, providing better outcomes for patients with diverse types of diabetes.
The Role of Research and Future Directions in Diabetes Management
Research in diabetes management is rapidly evolving, fostering advancements in technology and treatment protocols. Continuous glucose monitoring, insulin delivery systems, and collaborative care models are being developed to enhance patient care and improve glycemic control. Ongoing studies aim to identify the best approaches for integrating lifestyle interventions with pharmacotherapy to create personalized diabetes management plans.
Furthermore, the move towards precision medicine—tailoring healthcare based on individual variability—holds promise for improving diabetes care. Genetic research and advancements in biomarker identification may enable healthcare providers to develop more targeted therapies, fundamentally changing the treatment landscape for diabetes in the future.
As we continue to learn about diabetes and its complexities, public health initiatives focused on prevention, early diagnosis, and comprehensive care models become increasingly important. Collaborative efforts involving education, lifestyle modifications, and innovative research will pave the way for improved health outcomes and quality of life for millions affected by diabetes worldwide.
In conclusion, understanding the spectrum of diabetes is critical for effective management, prevention, and support. Whether dealing with Type 1, Type 2, gestational, or other forms, recognizing the unique characteristics and challenges of each type can lead to better care and quality of life for those affected by this complex disease. With ongoing research and advancements in management strategies, we have a brighter future in the fight against diabetes.