# Navigating the Diabetes Landscape: Understanding Type 1, Type 2, and Gestational Diabetes Therapeutics
Diabetes mellitus is a complex disease that affects millions worldwide, presenting unique challenges for individuals diagnosed with this condition. Understanding the subtleties of Type 1, Type 2, and Gestational Diabetes is crucial for implementing effective therapeutic strategies. This article will navigate the diabetes landscape, shedding light on the various treatment modalities available, lifestyle modifications, and ongoing research aimed at improving the quality of life for those affected by this chronic condition.
Understanding Diabetes: An Overview
diabetes is primarily categorized into Type 1, Type 2, and Gestational Diabetes, each with distinct characteristics, causes, and treatment approaches. Type 1 Diabetes (T1D) is an autoimmune condition, typically diagnosed in children and young adults, where the immune system attacks and destroys insulin-producing beta cells in the pancreas. This results in an absolute insulin deficiency and necessitates lifelong insulin therapy.
Conversely, Type 2 Diabetes (T2D) is more prevalent and often develops later in life. It is characterized by insulin resistance, where the body’s cells no longer respond effectively to insulin. T2D is often associated with obesity, a sedentary lifestyle, and genetic factors. Gestational Diabetes occurs during pregnancy, where some women experience high blood sugar levels despite not having diabetes prior to their pregnancy. Understanding these distinctions is fundamental for both patients and healthcare providers in tailoring appropriate treatment and management strategies.
Type 1 Diabetes: Therapeutic Approaches and Innovations
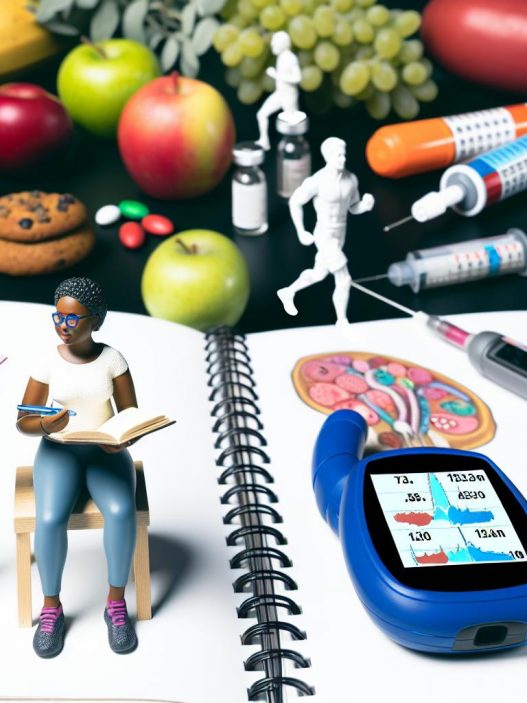
Management of Type 1 Diabetes has evolved significantly over the past few decades, primarily centered around insulin therapy. Patients must carefully monitor blood glucose levels and administer insulin multiple times a day, either through injections or via an insulin pump. Recent advancements have introduced technologies like continuous glucose monitors (CGMs), which provide real-time glucose readings and help patients make informed decisions regarding their insulin dosage.
In addition to insulin therapy, there is growing interest in adjunct therapies that aim to improve the overall management of T1D. For instance, the use of immunotherapies is being researched to prevent the autoimmune attack on beta cells. Current studies are exploring how medications can modify the immune response, potentially delaying or preventing the onset of T1D in those at high risk.
Moreover, lifestyle modifications remain a cornerstone of T1D management. A balanced diet, regular physical activity, and consistent blood sugar monitoring are vital components. Patients are encouraged to work closely with registered dietitians to create personalized meal plans that consider carbohydrate counting and glycemic index to maintain optimal blood sugar levels.
Type 2 Diabetes: Management and Prevention Strategies
Type 2 Diabetes management is often a multifaceted approach that focuses on lifestyle changes, medication, and regular monitoring of blood glucose levels. The cornerstone of T2D management is lifestyle modification, which includes adopting a healthy diet, engaging in regular physical activity, and achieving a healthy weight. Diet plays a significant role; studies indicate that foods low in carbohydrates and high in fiber can help stabilize blood sugar levels.
When lifestyle modifications alone are insufficient, medications may be introduced. Several classes of medications are available, including metformin, sulfonylureas, and SGLT2 inhibitors. Metformin is usually the first-line treatment, as it works to lower glucose production in the liver and improve insulin sensitivity in muscles. SGLT2 inhibitors have been gaining attention due to their ability to promote weight loss and reduce cardiovascular risk in T2D patients, making them a favorable option for many.
In recent years, advancements in diabetes technology, such as insulin pens, smart insulin pumps, and continuous glucose monitors (CGMs), have revolutionized how patients manage their diabetes. These devices offer better control and significantly reduce the risk of hypoglycemia. Therefore, regular monitoring of blood sugar levels remains crucial to ensure effective management of Type 2 Diabetes.
Gestational Diabetes: Risks, Management, and Treatment
Gestational Diabetes (GDM) is a condition that can occur during pregnancy, affecting about 2-10% of pregnant women. It arises when the body cannot produce enough insulin to maintain normal blood sugar levels, often exacerbated by hormonal changes associated with pregnancy. Women diagnosed with GDM must undergo rigorous monitoring to prevent complications for both mother and child.
Management strategies for GDM primarily focus on lifestyle modification, including diet and exercise, with the goal of maintaining blood glucose levels within recommended ranges. Registered dietitians often play an integral role in developing meal plans that ensure adequate nutrition while preventing excessive blood sugar spikes. Simple carb counting techniques and incorporating regular physical activity can greatly assist in achieving this goal.
In cases where lifestyle changes are insufficient, insulin therapy may be necessary. While some medications are contraindicated during pregnancy, insulin is considered safe and effective for managing GDM. Health care providers closely monitor both the mother’s and baby’s health throughout the pregnancy to prevent potential complications, including large birth weight and preeclampsia.
Collaborative Care: The Role of Healthcare Teams in Diabetes Management
Effective diabetes management significantly benefits from a collaborative approach between patients and healthcare teams, comprising endocrinologists, diabetes educators, registered dietitians, and mental health professionals. Each member plays a vital role in providing comprehensive care tailored to individual needs.
Endocrinologists specialize in diabetes management and are instrumental in developing treatment plans that align with current research and clinical practices. Conversely, diabetes educators offer invaluable support, empowering patients through education on self-management techniques, including medication adherence and lifestyle modifications.
Registered dietitians play a crucial part in helping patients understand the importance of nutrition in diabetes management. They work with patients to create meal plans that are not only balanced but also conducive to maintaining optimal blood glucose levels. Integrating mental health professionals becomes increasingly important as diabetes can take an emotional toll. Patients may face anxiety, depression, or burnout, emphasizing the need for holistic care that addresses both physical and emotional well-being.
Research and Future Directions in Diabetes Therapeutics
The landscape of diabetes therapeutics is continually evolving, thanks to ongoing research and innovations in treatment. Novel therapies currently under investigation include incretin-based therapies, gene therapy, and even potential vaccines to prevent or reverse diabetes. Incretin hormones play a crucial role in glucose metabolism, and drugs that mimic these hormones are showing promise in T2D management.
Additionally, gene therapy holds enormous potential in treating T1D by targeting the autoimmunity responsible for β-cell destruction. Research continues to evolve in this space, and while we are not yet at a point where gene therapy is widely available, clinical trials show valuable insights into its efficacy.
In recent years, the role of telemedicine in diabetes management has also gained traction, providing an effective means of ensuring ongoing patient education, monitoring, and support. Telehealth services enable patients to interact regularly with healthcare providers, ensuring that necessary adjustments to treatment plans can be made in real-time.
As research progresses, future therapeutic options will likely become more integrated, offering personalized care that adapts to the evolving needs of patients living with diabetes. With advancements in technology and an ever-expanding framework of collaborative care, the potential for improvements in diabetes management and patient outcomes is more promising than ever.
In conclusion, navigating the complex landscape of diabetes requires a comprehensive understanding of the various types and their distinct therapeutic approaches. By fostering collaboration among healthcare providers and patients and staying updated with ongoing research, effective management strategies can be developed to enhance the quality of life for individuals affected by Type 1, Type 2, and Gestational Diabetes. The road ahead is filled with the promise of innovation and improved outcomes for diabetes patients globally.