# Practical Tips for Managing Type 2 Diabetes Successfully
Managing Type 2 diabetes can be overwhelming, but with the right strategies and support, individuals can lead a healthy and fulfilling life. This blog aims to provide practical tips that can help anyone dealing with Type 2 diabetes to manage their condition effectively. From dietary changes and exercise routines to monitoring techniques, we will delve deeply into the essential practices that can make a significant impact on controlling blood sugar levels and enhancing overall well-being.
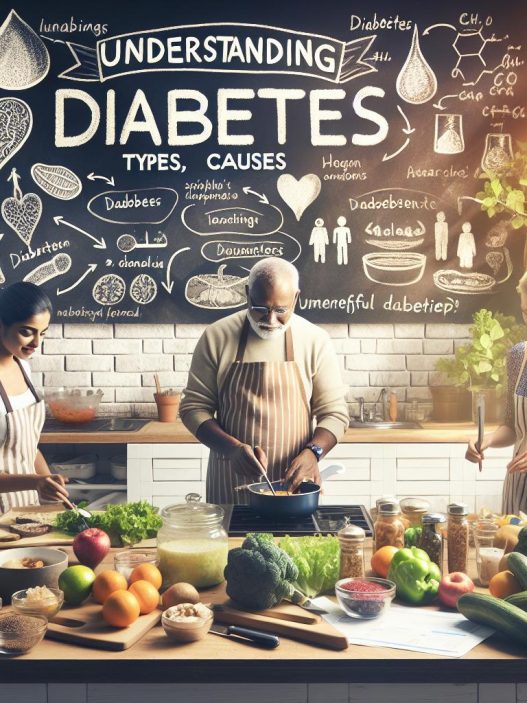
Understanding Type 2 Diabetes and Its Challenges
Type 2 diabetes is a chronic condition that affects the way your body metabolizes sugar (glucose). Unlike Type 1 diabetes, where the body produces little or no insulin, individuals with Type 2 diabetes may still produce insulin but their bodies do not respond effectively to it. This leads to a myriad of challenges including elevated blood sugar levels, which can result in various health complications over time. Recognizing the signs and understanding the implications of this condition is crucial. Symptoms may include increased thirst, frequent urination, fatigue, and blurred vision.
Effective management of Type 2 diabetes requires a comprehensive approach that encompasses lifestyle changes, medical interventions, and regular monitoring. A solid foundation of knowledge about the condition is essential for anyone navigating through it, as well as for the healthcare professionals supporting them. Familiarizing yourself with how diabetes impacts your body, potential long-term complications, and the importance of maintaining blood sugar levels can position you for successful management.
Adopting a Balanced and Healthy Diet
One of the most impactful ways to manage Type 2 diabetes is through a well-balanced diet tailored to your needs. It’s not just about cutting down on sugar but also about designing a meal plan that supports your energy levels and keeps blood glucose within a normal range. Incorporating a variety of foods, including whole grains, lean proteins, healthy fats, and fruits and vegetables, can help sustain metabolic health. Understanding the glycemic index of foods can further aid in meal planning, as it helps to identify which foods will cause more stable blood sugar increases versus those that cause rapid spikes.
Portion control is another crucial element in managing diabetes through diet. It’s important to be aware of serving sizes to avoid overeating, which can lead to undesirable blood sugar fluctuations. Consider using smaller plates or measuring portion sizes to manage intake effectively. Regular meal timings can also help maintain consistent blood sugar levels, so planning meals and snacks at specific times throughout the day is recommended. Strive to create colorful and diverse meals that are not only nutritious but also enjoyable, making it easier to stick to healthy eating habits in the long run.
Incorporating Physical Activity into Your Routine
Exercise plays a vital role in managing Type 2 diabetes as it helps to lower blood sugar levels and improve insulin sensitivity. Developing an exercise routine that you can realistically maintain is key. This could include activities such as walking, swimming, cycling, or any form of aerobic exercise that elevates your heart rate. Aim for at least 150 minutes of moderate aerobic activity per week, as recommended by health organizations, to reap the physiological benefits.
In addition to aerobic exercise, resistance training can also be incredibly beneficial for managing Type 2 diabetes. Incorporating strength training at least two to three times a week not only helps to build lean muscle mass but also improves metabolic rate, leading to better blood sugar control. If you find it challenging to initiate a workout routine, consider involving a friend or joining a class to create a motivational environment. Always consult with your healthcare provider before starting a new exercise program, especially if you have pre-existing health conditions.
Monitoring Blood Sugar Levels: Best Practices
Regular monitoring of blood sugar levels is an essential component of managing Type 2 diabetes. Understanding your blood sugar patterns enables you to make informed decisions about your diet, exercise, and medication. Use a glucometer to check your levels at different times of the day and record the results for your healthcare provider. This data can be invaluable during check-ups as it allows for adjustments to your management plan based on your specific needs.
Experience in monitoring your blood sugar helps in identifying triggers that may cause fluctuations. Keeping a daily log of food intake, physical activity, and blood sugar readings will illuminate patterns and trends over time. Additionally, Continuous Glucose Monitors (CGMs) are an excellent investment for those needing more regular monitoring as they provide real-time data and alerts for high or low blood sugars. Educate yourself about the importance of maintaining target ranges and how to respond to deviations effectively.
Working Collaboratively with Healthcare Professionals
Successful management of Type 2 diabetes often involves collaboration with various healthcare professionals. Regular appointments with an endocrinologist or primary care physician help to ensure that your management plan is on track and that you’re effectively addressing any areas of concern. Sometimes, a registered dietitian can provide personalized dietary advice tailored to your individual needs while offering guidance on meal planning and carbohydrate counting.
You might also want to connect with diabetes educators, who can teach you valuable skills in diabetes management and ensure you have the knowledge you need to make better choices. Support groups can also provide an emotional outlet and allow individuals with similar experiences to share tips and encouragement. The journey of managing Type 2 diabetes can feel isolating at times; having a network of support can help foster accountability and enthusiasm for pursuing a healthier lifestyle.
Managing Stress and Mental Well-being
Living with Type 2 diabetes can be stressful, as it requires continuous monitoring, decision-making, and lifestyle adjustments. Therefore, it’s incredibly important to prioritize mental well-being in your management plan. Chronic stress can negatively affect blood sugar levels, making it essential to find effective ways to manage stressors. Techniques such as mindfulness meditation, yoga, deep breathing exercises, and engaging in hobbies can alleviate stress and promote relaxation.
Connecting with others, whether through family, friends, or support groups, is also beneficial for mental health. Openly discussing your feelings and challenges can ease the burden and provide emotional relief. Setting realistic goals for your health journey is also crucial; remember that managing Type 2 diabetes is a marathon, not a sprint. Celebrate small victories along the way and stay motivated by focusing on the positives, such as improved health, increased energy, and a greater sense of well-being.
In conclusion, managing Type 2 diabetes effectively involves a multi-faceted approach that encompasses dietary changes, physical activity, regular monitoring, healthcare collaboration, and mental well-being. With commitment and the right strategies in place, individuals can successfully navigate their diabetes journey and lead a healthy, enjoyable life. As always, consult with your healthcare team for personalized recommendations and support tailored to your specific circumstances.