[ad_1]
Sure! Here’s an extensive blog post titled "Diabetes Explained: The Difference Between Type 1, Type 2, and Gestational Diabetes."
Introduction
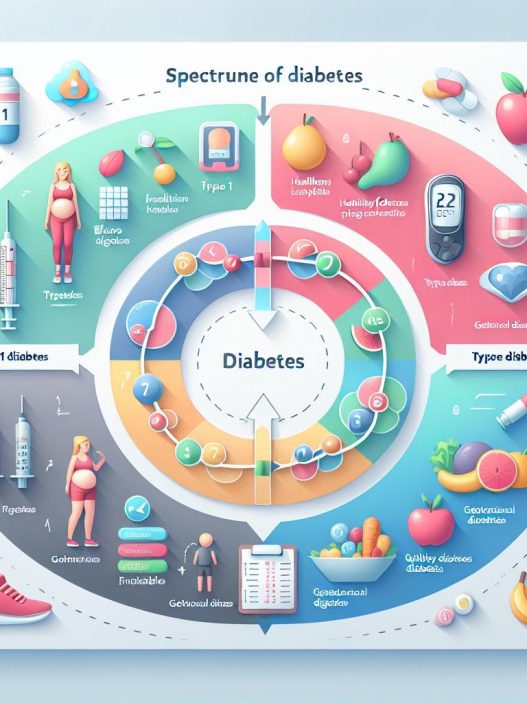
Diabetes is a chronic health condition that affects how your body turns food into energy. Understanding the distinctions among Type 1, Type 2, and Gestational Diabetes is essential for managing your health and making informed decisions. This comprehensive guide provides in-depth information about each type of diabetes, including symptoms, causes, risk factors, and management strategies to empower you in your journey to better health.
Understanding Diabetes: A Comprehensive Overview
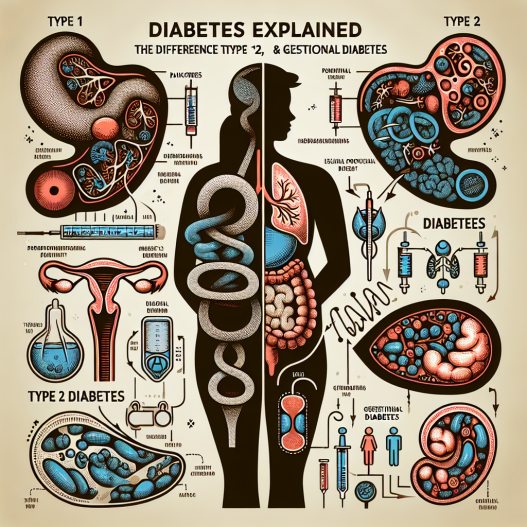
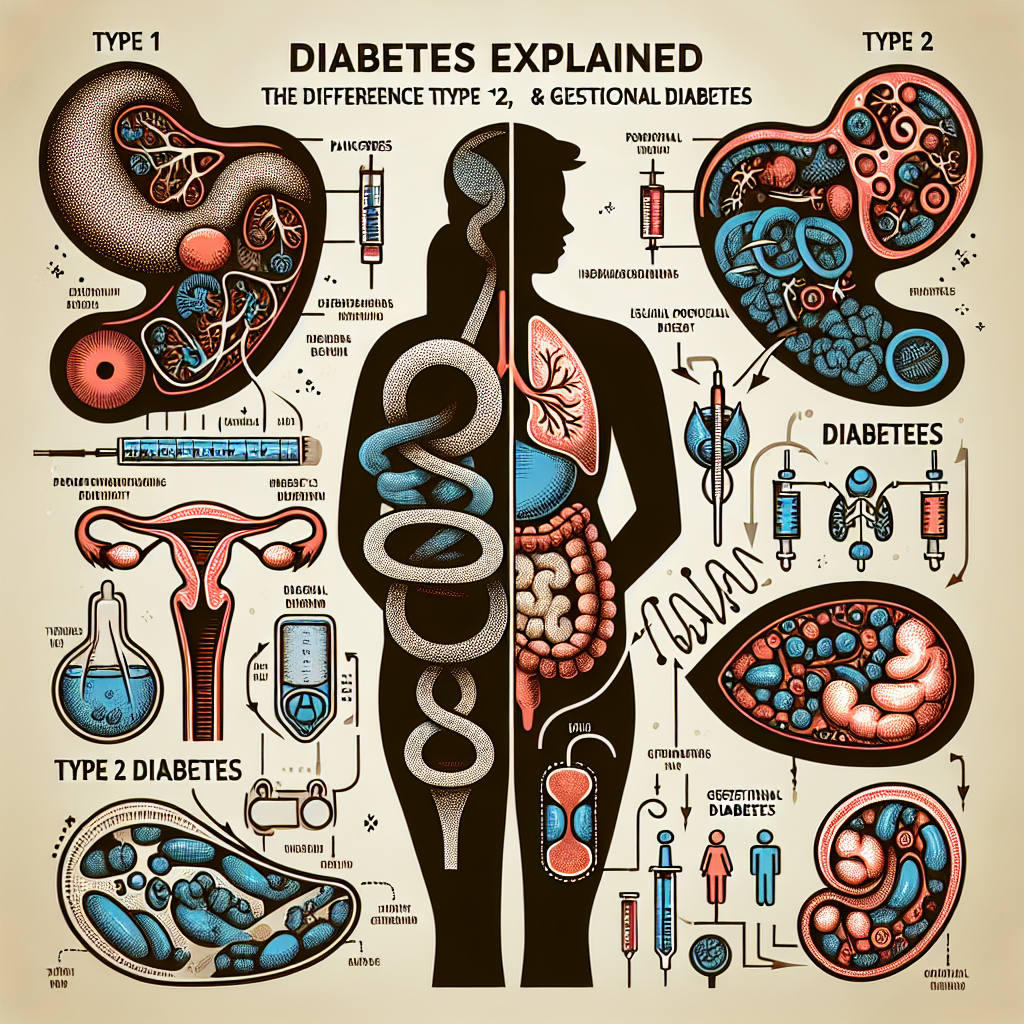
Diabetes is primarily classified into three main types: Type 1, Type 2, and Gestational Diabetes. Each type varies in its causes, symptoms, and management, making it vital to understand these differences for effective treatment and lifestyle adjustments. Type 1 Diabetes is an autoimmune condition where the body mistakenly attacks insulin-producing cells in the pancreas, resulting in little or no insulin production. This condition typically develops in children and young adults but can occur at any age.
On the other hand, Type 2 Diabetes is more prevalent and often associated with lifestyle factors such as obesity, physical inactivity, and poor diet. This form of diabetes involves insulin resistance, where the body does not effectively use insulin, leading to elevated blood glucose levels. In contrast, Gestational Diabetes occurs during pregnancy and usually resolves after childbirth, although it can increase the risk of developing Type 2 Diabetes later in life. Understanding these distinctions is crucial for managing symptoms and preventing complications.
Type 1 Diabetes: Causes, Symptoms, and Management
Type 1 Diabetes, previously known as juvenile diabetes, is characterized by the body’s inability to produce insulin. This autoimmune disorder occurs when the immune system attacks the pancreatic beta cells responsible for insulin production. Researchers believe that genetic predisposition, combined with environmental factors such as viral infections or other autoimmune issues, may trigger this condition. While the exact cause remains unclear, it’s evident that individuals with a family history of Type 1 Diabetes are at a higher risk.
Symptoms of Type 1 Diabetes often develop quickly and can include excessive thirst, frequent urination, extreme fatigue, weight loss, and blurred vision. Diagnosis typically involves blood tests to measure glucose levels and confirm the absence of insulin production. Once diagnosed, Type 1 Diabetes requires lifelong management through a combination of insulin therapy, regular blood glucose monitoring, and careful management of diet and physical activity. Education is also vital; understanding how foods affect blood glucose levels can empower individuals to make healthier choices.
Managing Type 1 Diabetes also involves staying vigilant about potential complications, including cardiovascular disease, nerve damage, and kidney damage. Regular check-ups and screenings are crucial for early detection and management of these complications. Stress management, maintaining a balanced diet, and engaging in regular physical activity can also improve overall health outcomes and enhance the quality of life for those with Type 1 Diabetes.
Type 2 Diabetes: Causes, Symptoms, and Lifestyle Management
Type 2 Diabetes is the most common form of the condition, accounting for roughly 90-95% of all diabetes cases. Unlike Type 1, this form usually develops in adults, largely due to a combination of genetic and lifestyle factors. Obesity is a significant risk factor, as excess weight can lead to insulin resistance. Factors such as age, familial history, sedentary lifestyle, and an unhealthy diet further increase the likelihood of developing Type 2 Diabetes.
Common symptoms include increased thirst, frequent urination, fatigue, blurred vision, and slow-healing wounds. However, many individuals may be unaware they have the condition due to mild or no symptoms. Diagnosis involves blood tests to measure fasting glucose levels or an HbA1c test to assess average blood glucose over three months. Early detection is crucial for effective management and can be achieved through regular health check-ups, particularly for individuals at risk.
Managing Type 2 Diabetes often involves lifestyle modifications, including weight loss, a balanced diet rich in whole grains, fruits, vegetables, lean proteins, and regular physical activity. Monitoring blood glucose levels is essential for understanding how different foods and activities affect your body. In some cases, medication may be required to help manage blood sugar levels effectively. Understanding your body’s needs and building healthy habits can significantly improve your overall health and well-being.
Gestational Diabetes: Exploring Causes and Management Strategies
Gestational Diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased needs of both mother and baby. While the exact cause is unknown, hormonal changes, genetic factors, and excess weight before pregnancy contribute to insulin resistance. This type of diabetes typically develops in the second or third trimester and can increase risks for both mother and child if not managed effectively.
Symptoms of Gestational Diabetes are often mild or absent, making routine screening crucial for pregnant women. Healthcare providers usually conduct glucose screening tests between 24 and 28 weeks of pregnancy. If diagnosed, management may include dietary modifications, regular physical activity, and, in some cases, insulin therapy. Maintaining blood sugar levels within the target range is essential to minimize risks such as preeclampsia, cesarean delivery, and complications for the baby.
Post-pregnancy, women with Gestational Diabetes are at an increased risk for developing Type 2 Diabetes later in life. Therefore, continuing to monitor blood sugar levels and pursuing a healthy lifestyle is crucial. Educational resources and support groups can provide valuable guidance on maintaining optimal health, ultimately benefiting both mothers and their children.
Common Myths About Diabetes: Debunking Misconceptions
There are numerous misconceptions about diabetes that can hinder public understanding and managing the condition effectively. One common myth is that diabetes only affects individuals who are overweight or lead a sedentary lifestyle. While these factors increase the risk of Type 2 Diabetes, it’s important to note that Type 1 Diabetes can develop in individuals of any body type, often in childhood or young adulthood. Awareness of these differences is crucial for advancing public education and reducing stigma surrounding the disease.
Another prevalent myth is that people with diabetes cannot consume sugar. While it’s essential to monitor carbohydrate intake, individuals with diabetes can still enjoy sweets in moderation. Managing diabetes effectively is about balancing carbohydrate intake, understanding dietary choices, and maintaining a healthy lifestyle rather than completely eliminating certain foods. Education on glycemic index, portion control, and making informed choices empowers individuals with diabetes to manage their health without depriving themselves.
Additionally, many people believe that diabetes is a disease that only requires medication to manage, neglecting the importance of lifestyle changes. A nutritious diet and physical activity play crucial roles in diabetes management. Even with medication, lifestyle choices can significantly impact blood sugar levels and overall health. Recognizing the importance of these factors can help individuals adopt a more holistic approach to managing their diabetes.
The Role of Support Systems in Diabetes Management
Managing diabetes can often be overwhelming, but having a supportive network can make a significant difference. Family members, friends, and healthcare providers play essential roles in providing encouragement and assistance in navigating the complexities of diabetes management. Emotional support can help individuals adhere to their treatment plans and cope with the various challenges that diabetes presents.
Joining diabetes support groups can also provide valuable resources, insights, and camaraderie. Sharing experiences with others who face similar struggles can foster feelings of connection and reduce feelings of isolation. Health professionals specializing in diabetes education can offer personalized guidance, helping individuals develop a comprehensive plan tailored to their needs. This support can include nutritional counseling, stress management techniques, and strategies for effective glucose monitoring.
Moreover, technology has increasingly become an ally in diabetes management. Mobile apps and continuous glucose monitors (CGMs) enhance access to critical data, enabling individuals to make informed decisions about their health. Embracing a support system that leverages both personal connections and technological aids can significantly improve the quality of life for individuals living with diabetes.
This post is designed to provide a comprehensive understanding of the differences and similarities between Type 1, Type 2, and Gestational Diabetes. By addressing various aspects of diabetes, such as symptoms, causes, management strategies, misconceptions, and support systems, this content aims to empower readers with the knowledge to manage their health effectively. If you want to enhance specific areas further or add more content, feel free to let me know!
[ad_2]