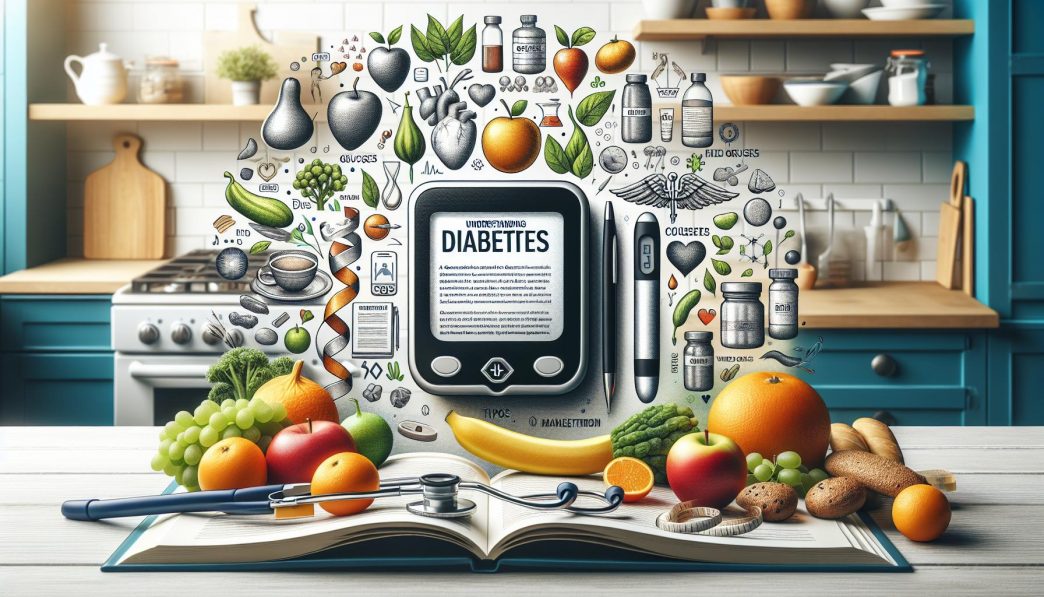
# Understanding Diabetes: A Comprehensive Guide to Types, Causes, and Management
Diabetes is a complex and chronic health condition that affects millions of people around the world. With rising prevalence rates, understanding diabetes is crucial for prevention and effective management. This comprehensive guide will delve into the types of diabetes, the factors contributing to its development, and the best strategies for management. By acquiring knowledge about diabetes, individuals can empower themselves and their loved ones to live healthier lives.
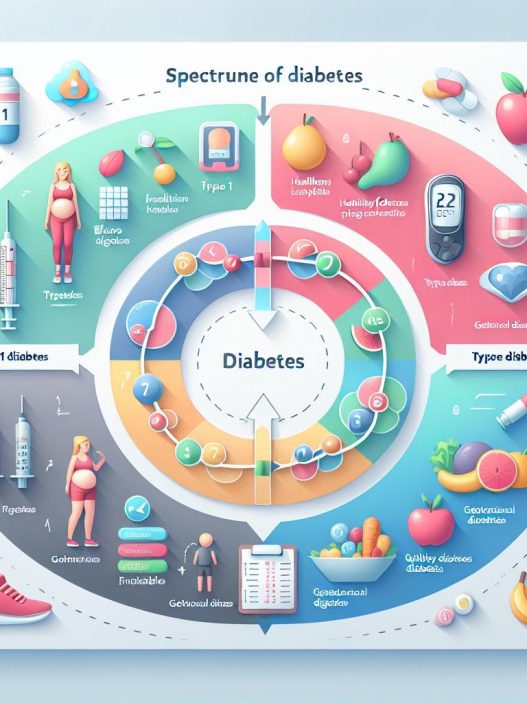
Understanding the Different Types of Diabetes
Diabetes is primarily classified into two main types: Type 1 diabetes and Type 2 diabetes. Both types involve issues with insulin, the hormone that regulates blood sugar levels; however, they differ significantly in their causes, development, and management strategies.
Type 1 diabetes is an autoimmune condition that typically manifests early in life. In individuals with Type 1 diabetes, the immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to an absolute deficiency of insulin, making individuals reliant on external insulin administration for survival. Symptoms often arise quickly, and lifelong management is essential.
In contrast, Type 2 diabetes, which accounts for approximately 90-95% of diabetes cases, usually develops later in life and is characterized by insulin resistance. This means that while the pancreas produces insulin, the body’s cells do not respond effectively to it, leading to elevated blood sugar levels. Risk factors include obesity, poor diet, physical inactivity, and genetic predisposition. Onset may be gradual, often going unnoticed in the early stages, making understanding and early detection paramount.
Causes of Diabetes: Unraveling the Risk Factors
The causes of diabetes are multifaceted, involving a combination of genetic, environmental, and lifestyle factors. Understanding these variables can help in identifying at-risk individuals and implementing preventive measures.
Genetics play a significant role in the predisposition to diabetes. Family history of the disease increases the likelihood of developing Type 2 diabetes, particularly among first-degree relatives. Specific genetic mutations also contribute to Type 1 diabetes, although environmental factors such as viral infections may trigger its onset.
Lifestyle choices significantly impact the risk of developing diabetes. A sedentary lifestyle, characterized by insufficient physical activity, contributes to weight gain and obesity—major risk factors for Type 2 diabetes. Furthermore, dietary habits, such as high consumption of sugary beverages, processed foods, and unhealthy fats, can lead to insulin resistance. Stress and inadequate sleep have also been implicated in increasing diabetes risk, highlighting the importance of holistic well-being.
Recognizing the Symptoms of Diabetes
Early recognition of diabetes symptoms is critical for timely management and to prevent complications. While symptoms can vary depending on the type of diabetes, there are several common warning signs to be aware of.
In Type 1 diabetes, symptoms can develop quickly and may include excessive thirst, frequent urination, extreme fatigue, blurred vision, and unintentional weight loss. These can often be mistaken for other illnesses, which makes awareness crucial for early detection and treatment.
Type 2 diabetes symptoms tend to develop more gradually and can be subtle. Common symptoms include increased thirst, frequent urination, slow-healing sores, and dark patches on the skin known as acanthosis nigricans. Many individuals with Type 2 diabetes may experience no symptoms at all, underscoring the importance of regular screening, especially for those with risk factors.
Complications of Diabetes: The Importance of Management
Managing diabetes effectively is essential to avoid serious complications that can severely impact quality of life. Uncontrolled diabetes can lead to both acute and chronic complications affecting various organ systems.
Acute complications of diabetes include hypoglycemia (low blood sugar) and hyperglycemia (high blood sugar). Hypoglycemia can result in dizziness, confusion, and even loss of consciousness if not treated promptly. Conversely, prolonged hyperglycemia can lead to diabetic ketoacidosis (DKA), a life-threatening condition primarily seen in Type 1 diabetes that requires immediate medical intervention.
Chronic complications of diabetes develop over time and can affect the heart, kidneys, eyes, and nervous system. Cardiovascular diseases, such as heart attack and stroke, are more prevalent in diabetics. Diabetic nephropathy can lead to kidney failure, necessitating dialysis or transplantation. Diabetic retinopathy can cause vision impairment and blindness, highlighting the importance of regular eye exams for individuals with diabetes. Peripheral neuropathy can lead to pain, tingling, and even amputation in severe cases.
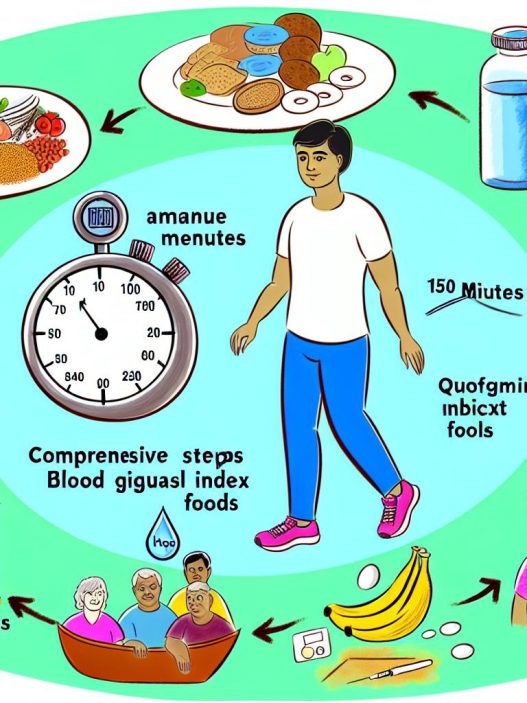
Effective Management Strategies for Diabetes
A comprehensive management plan for diabetes should encompass lifestyle modifications, medication, regular monitoring, and education. These combined strategies are crucial for achieving optimal blood sugar control and preventing complications.
Lifestyle changes form the cornerstone of diabetes management. A balanced diet rich in whole grains, lean proteins, healthy fats, and plenty of fruits and vegetables should replace processed foods high in sugar and unhealthy fats. Regular physical activity, such as brisk walking, cycling, or swimming, not only assists in maintaining a healthy weight but also enhances insulin sensitivity. Stress management techniques, including mindfulness and yoga, can further support overall well-being.
Medications for diabetes management vary between individuals and may include oral hypoglycemics or insulin therapy. Monitoring blood glucose levels regularly is essential to assess treatment efficacy and make necessary adjustments. Education is also paramount, empowering patients with the knowledge and skills needed to manage their condition effectively. Support from healthcare providers, diabetes educators, and support groups can facilitate this journey.
Understanding diabetes and its complexities is vital for individuals living with the condition and their support networks. By gaining knowledge about the types, causes, symptoms, and management strategies, individuals can take control of their health and live fulfilling lives despite the challenges of diabetes. It is a journey that requires commitment, but with the right tools and resources, managing diabetes is not only possible but can also lead to better health outcomes and a higher quality of life.
In conclusion, the importance of awareness and education regarding diabetes cannot be overstated. As this chronic condition continues to impact millions, a comprehensive understanding serves as the foundation for prevention, early detection, and effective management strategies that enhance the well-being of individuals affected by diabetes.