# Understanding Diabetes: A Comprehensive Guide to Types, Causes, and Treatments
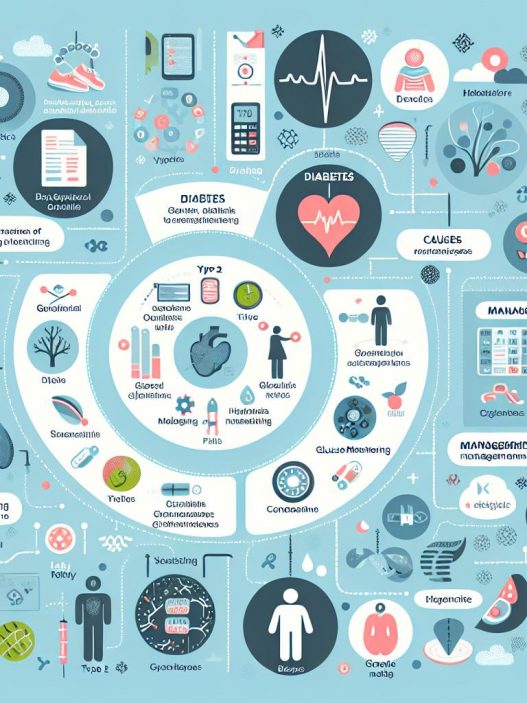
Diabetes is a chronic illness that affects millions of people worldwide, posing serious health risks if left unmanaged. This comprehensive guide aims to shed light on the different types of diabetes, their causes, available treatments, and management strategies. By understanding diabetes better, individuals can make informed health decisions, ultimately enhancing their quality of life.
Types of Diabetes: A Detailed Exploration
Diabetes is primarily categorized into several types, each with unique characteristics, causes, and implications. The two most common forms are Type 1 and Type 2 diabetes, but gestational diabetes and other less common types also warrant attention.
Type 1 diabetes, often diagnosed in children and young adults, is an autoimmune condition where the body’s immune system attacks insulin-producing beta cells in the pancreas. This destruction leads to little or no insulin production, necessitating lifelong insulin therapy for management. Individuals with Type 1 diabetes must regularly monitor their blood sugar levels and administer insulin injections or utilize an insulin pump to maintain optimal blood glycemic control.
On the other hand, Type 2 diabetes is characterized by insulin resistance and is more prevalent among adults, especially in those who are overweight or lead sedentary lifestyles. Unlike Type 1 diabetes, those with Type 2 diabetes can produce insulin, but their bodies cannot effectively use it. This insufficiency often prompts a range of treatments, including lifestyle modifications like diet and exercise, as well as medications to enhance insulin sensitivity or increase insulin production.
Causes of Diabetes: Understanding the Risk Factors
Understanding the causes and risk factors associated with diabetes is pivotal for prevention and management. Genetic and lifestyle factors play a significant role in the development of this chronic disease. Family history is a crucial factor, as having a parent or sibling with diabetes can significantly increase your risk. Genetic predisposition, combined with environmental influences, creates a perfect storm for the development of diabetes.
Nutrition and physical activity level also have profound consequences on diabetes risk. Diets high in refined sugars and unhealthy fats can elevate blood sugar levels, while regular physical activity helps maintain a healthy weight and improve insulin sensitivity. Additionally, other factors such as age, ethnicity, stress, hormonal changes, and certain medical conditions can also contribute to the development of diabetes.
Moreover, gestational diabetes, which affects pregnant women, requires special consideration. Hormonal changes during pregnancy can lead to insulin resistance. Women who have gestational diabetes are at an increased risk of developing Type 2 diabetes later in life, highlighting the importance of lifestyle modifications and follow-up care postpartum.
Symptoms and Diagnosis: Recognizing Diabetes Early
Early detection of diabetes is crucial for effective management and reducing the risk of complications. Common symptoms of diabetes include increased thirst, frequent urination, extreme fatigue, blurred vision, and slow healing of wounds. Some people may also experience unexplained weight loss, which is particularly common in individuals with Type 1 diabetes due to the lack of insulin.
Diagnostic methods for diabetes include fasting blood glucose tests, oral glucose tolerance tests (OGTT), and hemoglobin A1c tests. The fasting blood glucose test measures blood sugar levels after an overnight fast, while the OGTT evaluates how the body processes glucose after fasting and receiving a sugary drink. The A1c test reflects average blood glucose levels over the previous two to three months. Consistent elevation in these tests can result in a diabetes diagnosis.
It is essential to visit healthcare professionals if you exhibit any symptoms or are at risk due to family history or lifestyle factors. Early diagnosis and intervention can significantly improve long-term health outcomes and minimize complications associated with untreated diabetes.
Treatment Options for Diabetes: A Comprehensive Overview
The management of diabetes requires a multifaceted approach tailored to the individual’s specific needs. Treatment for Type 1 diabetes primarily revolves around insulin therapy, with the goal being to mimic the pancreas’s natural insulin release. Patients must develop a routine to monitor their blood glucose levels and adjust their insulin doses accordingly.
For Type 2 diabetes, the treatment plan may include lifestyle changes, such as adopting a balanced diet rich in whole grains, fruits, vegetables, and lean protein. Regular physical activity is equally important, as it helps regulate blood sugar levels and promotes overall well-being. In addition to lifestyle modifications, many individuals with Type 2 diabetes may require medications. These can include metformin, sulfonylureas, or newer classes of drugs like GLP-1 receptor agonists, which help improve blood sugar control.
Moreover, diabetes management is not solely about medication and lifestyle changes. Education and emotional support are critical components of effective diabetes management. Engaging with healthcare teams, enrolling in diabetes education programs, and seeking psychological support can empower individuals to take an active role in their health management journey. This holistic approach significantly improves quality of life and can lead to better health outcomes.
Complications of Diabetes: Understanding the Risks
If poorly managed, diabetes can lead to a myriad of serious complications affecting various organs and bodily systems. Some of the most common complications are cardiovascular disease, nerve damage, kidney damage, eye damage, and foot complications. Individuals with diabetes are at a higher risk of developing heart disease, stroke, and hypertension due to deteriorated blood vessels and increased blood sugar levels.
Neuropathy, or nerve damage, often manifests as numbness, tingling, and pain in the extremities. This condition can lead to a loss of sensation, making it difficult for individuals to notice injuries or infections that can worsen over time. Renal complications, such as diabetic nephropathy, can lead to kidney failure, requiring dialysis or a kidney transplant in severe cases.
Diabetes can also impact vision, leading to diabetic retinopathy, macular edema, or even blindness if not properly managed. Regular eye examinations are essential for individuals with diabetes to catch any potential issues early. Lastly, poor circulation and nerve damage can increase the risk of foot ulcers and infections, sometimes necessitating amputations in severe cases.
Taking proactive measures to mitigate these risks is essential. This involves maintaining strict blood sugar control, regular medical check-ups, and living a healthy lifestyle to protect against the severe complications of diabetes.
Living with Diabetes: Best Practices for Everyday Management
Living with diabetes requires a commitment to consistent self-care and management practices. Individuals should establish a comprehensive routine that includes regular monitoring of blood glucose levels, adhering to prescribed medication regimens, and maintaining a balanced diet. Carbohydrate counting and understanding glycemic index can aid in making better food choices, ultimately helping regulate blood sugar levels more effectively.
Support from healthcare professionals, family, and friends plays a crucial role in the successful management of diabetes. Joining support groups or connecting with others living with diabetes can provide practical insights on coping strategies, sharing experiences, and fostering a sense of community.
Additionally, incorporating physical activity into daily routines can immensely benefit diabetes management. Engaging in regular exercise not only helps to control blood sugar levels but also contributes to weight management, lowers stress levels, and promotes overall cardiovascular health. Creating an activity plan that includes enjoyable exercises can lead to sustainable lifestyle changes.
In conclusion, understanding diabetes, recognizing its symptoms, learning about treatment options, and embracing lifestyle changes ultimately lead to a healthier life. Awareness and education are key in empowering individuals to take charge of their diabetes management journey. Emphasizing the interconnectedness of diet, exercise, medication adherence, and emotional support will pave the way for effective diabetes management and improved overall health.