# Understanding the Spectrum: A Comprehensive Guide to Type 1, Type 2, and Gestational Diabetes
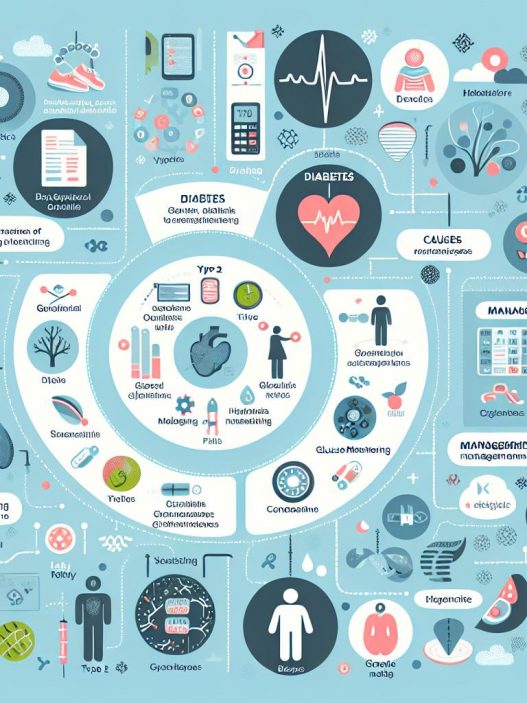
Diabetes is a complex and prevalent condition affecting millions of individuals worldwide. Understanding the spectrum of diabetes is crucial for management and prevention. This comprehensive guide delves into the intricacies of Type 1, Type 2, and Gestational Diabetes, unraveling their differences, symptoms, treatment options, and preventative measures. By the end of this article, you’ll gain a thorough understanding of these three main types of diabetes, empowering you to make informed health decisions.
Understanding Type 1 Diabetes: Causes, Symptoms, and Management
Type 1 Diabetes (T1D) is often diagnosed in childhood or adolescence, although it can occur at any age. It is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to an absolute lack of insulin, a hormone crucial for converting glucose from food into energy. The exact cause of this autoimmune response remains largely unknown, but genetic and environmental factors likely play a significant role.
Recognizing the symptoms of Type 1 Diabetes is critical for early diagnosis and management. Common symptoms include increased thirst, frequent urination, extreme hunger, weight loss, fatigue, and blurred vision. If left unchecked, Type 1 diabetes can lead to serious complications such as diabetic ketoacidosis (DKA), a life-threatening condition resulting from a significant lack of insulin. Management of T1D requires lifelong insulin therapy, which can be administered through injections or an insulin pump, along with a balanced diet and regular blood sugar monitoring.
Exploring Type 2 Diabetes: Risk Factors, Symptoms, and Treatment Options
Type 2 Diabetes (T2D) is the most common form of diabetes, usually developing in adults, although it is increasingly being diagnosed in children and adolescents due to rising obesity rates. Unlike Type 1, T2D is characterized by insulin resistance, where the body does not use insulin efficiently, and a gradual decline in insulin production. Multiple risk factors contribute to T2D, including obesity, age, sedentary lifestyle, and a family history of diabetes. Recognizing these risk factors is essential for early intervention and prevention.
The symptoms of Type 2 Diabetes can be subtle and may develop gradually over time. They include increased thirst and hunger, frequent urination, fatigue, blurred vision, and slow-healing sores or frequent infections. It’s common for individuals with T2D to be unaware of their condition until routine blood tests reveal elevated glucose levels. For management, lifestyle changes—such as adopting a healthy diet, regular physical activity, and weight loss—are vital. In more advanced cases, medical treatments like oral medications or insulin therapy may be necessary to maintain blood glucose levels within a target range.
Gestational Diabetes: Understanding the Condition and Its Impact
Gestational Diabetes Mellitus (GDM) is a type of diabetes that develops during pregnancy, typically occurring in the second or third trimester. It affects approximately 2-10% of pregnant women and can pose risks to both the mother and the developing fetus. The body’s insulin production cannot keep up with the increased demands during pregnancy, leading to elevated blood glucose levels. Understanding GDM is pivotal for both immediate health management and long-term considerations.
Symptoms of gestational diabetes are often nonexistent, which is why screening is usually performed between the 24th and 28th weeks of pregnancy. Risk factors include overweight or obesity, polycystic ovary syndrome (PCOS), having a family history of diabetes, and being over the age of 25. If not managed properly, GDM can lead to complications such as excessive birth weight, premature delivery, and a heightened risk of Type 2 Diabetes for both mother and child post-pregnancy. Treatment primarily involves dietary changes, physical activity, and sometimes insulin therapy to help manage blood glucose levels throughout pregnancy.
The Intersection of Diabetes Types: Commonalities and Differences
While Type 1, Type 2, and Gestational Diabetes are distinct conditions, they share common themes regarding glucose management and the importance of maintaining healthy blood sugar levels. One of these commonalities is the significance of lifestyle choices in managing all types of diabetes. Healthy eating patterns, regular exercise, and routine monitoring of blood glucose play critical roles across the board. Additionally, education and support systems, including healthcare professionals and diabetes support groups, are essential for fostering effective management strategies.
Differences among these types predominantly revolve around their underlying causes and demographics affected. Type 1 Diabetes is mainly characterized as an autoimmune disorder that typically arises in younger populations, while Type 2 Diabetes is primarily linked to lifestyle factors and commonly develops in adults. Gestational Diabetes, unique to pregnancy, requires specific management techniques to ensure the health of both mother and baby. Understanding these distinctions aids in the development of targeted interventions and highlights the importance of personalized diabetes care.
Preventative Strategies: Can Diabetes Be Avoided?
Preventative strategies play a vital role in the fight against Type 2 Diabetes, with lifestyle modifications offering substantial promise in reducing risk factors. Maintaining a healthy weight is the most significant prevention strategy, as even modest weight loss can improve insulin sensitivity and glucose management. Regular physical activity is crucial; engaging in at least 150 minutes of moderate aerobic exercise each week can help diminish the risk and improve overall health.
Dietary modifications, such as adopting a balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats, can further promote healthy blood sugar levels. Reducing sugar and refined carbohydrates is also essential, as these can cause rapid spikes in blood sugar. For women who have experienced Gestational Diabetes, maintaining a healthy lifestyle post-pregnancy is critical in minimizing the risk of developing Type 2 Diabetes in the future.
Living with Diabetes: Ongoing Management and Support
Living with any form of diabetes necessitates ongoing management and a robust support system. For those diagnosed with Type 1 or Type 2 diabetes, frequent blood sugar monitoring can help ensure that levels remain within a target range. For those with Type 1, this often means multiple daily injections or the use of an insulin pump, while individuals with Type 2 may manage their condition through oral medications or lifestyle adjustments.
Emotional and psychological support is equally important for individuals living with diabetes. Dealing with a chronic condition can be challenging, and many find that connecting with support groups—either online or in person—can provide a sense of understanding and camaraderie. Mental health resources are also valuable, as anxiety and depression can be common among those managing diabetes, affecting overall well-being and adherence to treatment plans.
—
In conclusion, understanding diabetes—from Type 1 through Gestational Diabetes—encompasses learning about its various forms, symptoms, and management strategies. Equipped with this knowledge, individuals can cultivate effective prevention and management practices, fostering a healthier future free from the complications associated with diabetes. Whether you are managing diabetes yourself or seeking to support a loved one, comprehensive awareness and compassionate care are essential in navigating this spectrum of health.