# Understanding the Spectrum of Diabetes: A Comprehensive Guide to Type 1, Type 2, and Gestational Diabetes
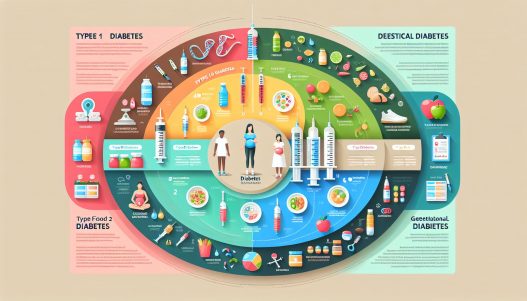
Diabetes is a complex group of diseases affecting how the body uses blood sugar (glucose). Understanding the spectrum of diabetes is crucial for prevention, management, and knowing the differences between Type 1, Type 2, and gestational diabetes. This comprehensive guide aims to provide in-depth knowledge about each type of diabetes, their symptoms, risk factors, treatments, and lifestyle adjustments necessary for managing these conditions effectively.
Understanding Type 1 Diabetes: An Immune Response
Type 1 diabetes, often diagnosed in children and young adults, occurs when the immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This autoimmune disorder results in little to no insulin production, necessitating lifelong insulin therapy for affected individuals. The exact cause remains unclear, but genetic and environmental factors are thought to contribute to the risk of developing Type 1 diabetes.
Symptoms of Type 1 diabetes can manifest suddenly and may include excessive thirst, frequent urination, extreme hunger, unintended weight loss, fatigue, and blurred vision. Given the abrupt nature of its onset, it’s imperative for those experiencing symptoms to seek medical attention promptly. Although there is no known way to prevent Type 1 diabetes, research continues to explore potential immunotherapeutic approaches to modify the disease’s course or prevent its onset in genetically predisposed individuals.
Management of Type 1 diabetes centers around regular insulin administration, blood glucose monitoring, and carbohydrate counting. Continuous glucose monitors and insulin pumps are advanced technologies that offer improved flexibility and blood sugar control. Moreover, awareness of hypoglycemia (low blood sugar) and its symptoms is critical, as individuals with Type 1 diabetes are at heightened risk for severe episodes that require timely intervention.
A Deep Dive into Type 2 Diabetes: The Most Common Form
Type 2 diabetes accounts for approximately 90-95% of diabetes cases and is predominantly characterized by insulin resistance and relative insulin deficiency. Unlike Type 1 diabetes, where insulin production is almost nonexistent, individuals with Type 2 diabetes often produce adequate amounts of insulin but their bodies cannot use it effectively. While typically diagnosed in adults, an alarming rise in cases among children and adolescents, often related to obesity and sedentary lifestyles, has been observed.
The development of Type 2 diabetes is gradual, making its symptoms easy to overlook. Common signs include increased thirst, frequent urination, extreme fatigue, blurred vision, and slow-healing sores. As symptoms may not be pronounced initially, regular screening is essential, especially for individuals at higher risk due to factors like obesity, family history, or age.
Managing Type 2 diabetes revolves around lifestyle modifications, such as adopting a balanced diet, exercising regularly, and achieving a healthy weight. Medications may also be prescribed to help control blood sugar levels, ranging from metformin to newer classes of drugs that enhance insulin secretion or increase insulin sensitivity. In some cases, individuals may require insulin therapy. Understanding the implications of Type 2 diabetes is vital, as it significantly raises the risk of multiple health complications, including heart disease, kidney damage, nerve problems, and vision issues.
Gestational Diabetes: Navigating Diabetes During Pregnancy
Gestational diabetes occurs during pregnancy when the body cannot produce enough insulin to meet the increased demands, resulting in elevated blood sugar levels. It typically develops around the 24th week of pregnancy and can have significant implications for both the mother and the baby if not managed effectively. Pregnant individuals should be screened for gestational diabetes during routine prenatal visits, particularly if they exhibit risk factors such as obesity or a family history of diabetes.
The symptoms of gestational diabetes are often subtle, and in many cases, women may not exhibit any noticeable symptoms. However, increased thirst and frequent urination may occur. It is crucial to monitor blood sugar levels and receive prompt treatment to reduce potential complications, which can include high birth weight for the baby, preterm birth, and increased risk of developing Type 2 diabetes later in life for both mother and child.
Management of gestational diabetes typically involves dietary modifications, physical activity, and regular blood-glucose monitoring. A dietitian may help design a meal plan that ensures adequate nutrition for both mother and baby while maintaining stable blood sugar levels. In some cases, insulin therapy or oral medications may be necessary to achieve optimal control. Post-delivery, women are advised to undergo screening for Type 2 diabetes, as those with a history of gestational diabetes are at increased risk for developing it.
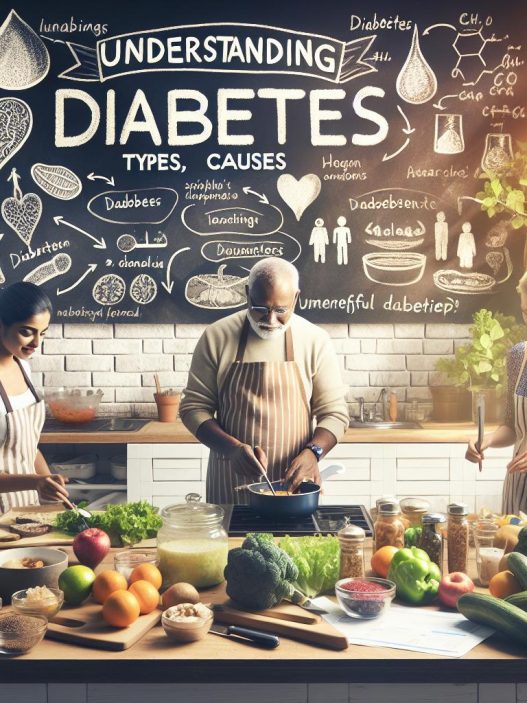
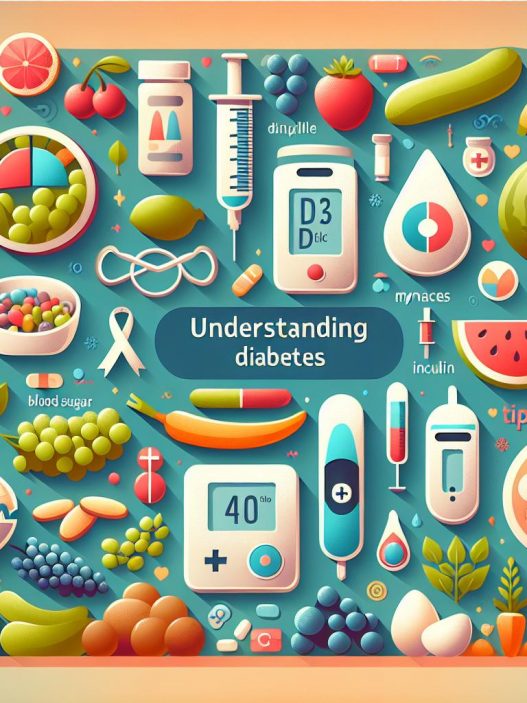
The Importance of Nutrition in Diabetes Management
Nutrition plays a pivotal role in managing all forms of diabetes. A balanced diet can help control blood sugar levels, manage weight, and reduce the risk of diabetes-related complications. Carbohydrate intake, particularly, requires careful monitoring, as carbohydrates have the most significant impact on blood glucose levels. Individuals with diabetes should focus on consuming whole grains, fruits, vegetables, lean proteins, and healthy fats to maintain overall health and stable blood sugar levels.
Meal planning is essential for those managing diabetes. This involves understanding portion sizes, nutrient timing, and how various foods affect blood sugar. Consuming foods high in fiber can help slow glucose absorption and prevent spikes in blood sugar after meals. Moreover, individuals should limit their intake of simple sugars and processed foods, which can hastily escalate blood glucose levels.
Additionally, hydration is often underrated in diabetes management. Proper hydration helps maintain overall health and can assist in managing blood sugar levels. Sugary drinks should be replaced with water or unsweetened beverages whenever possible to avoid unnecessary calorie intake and blood sugar surges. Collaborating with a registered dietitian can provide tailored guidance suited to individual needs, preferences, and specific diabetes management goals.
Exercise: A Key Component of Diabetes Management
Physical activity is a cornerstone of diabetes management and offers numerous benefits, including improved insulin sensitivity, enhanced mood, and weight management. Regular exercise helps individuals better regulate their blood sugar levels, ultimately reducing the risk of complications associated with diabetes. Activities can range from moderate aerobic exercises like walking or cycling to strength training and flexibility exercises like yoga.
For individuals with diabetes, it is essential to work with healthcare providers to create a safe and effective exercise plan. Monitoring blood sugar before and after exercise is crucial to avoid hypo or hyperglycemia. Certain precautions should be taken, such as having quick sources of carbohydrates on hand and understanding how different types of exercise affect blood sugar levels.
Additionally, incorporating physical activity into daily routines can be beneficial. This might involve taking the stairs instead of the elevator, walking during breaks, or engaging in active hobbies. The goal is not only to achieve a fit lifestyle but also to build a sustainable routine that maintains enjoyment and minimizes burnout. A supportive community or engaging others in physical activities can enhance motivation and adherence to exercise regimens.
Conclusion: A Holistic Approach to Diabetes Management
Understanding the spectrum of diabetes is vital for those diagnosed with the condition and for their loved ones. A comprehensive approach that addresses medical, dietary, and lifestyle factors is essential in managing diabetes effectively. Education plays a crucial role, empowering individuals with the knowledge needed to navigate their diabetes experience, recognize symptoms of health complications, and engage in proactive self-care.
Moreover, ongoing research into diabetes treatment, prevention, and management continues to evolve. From innovative medications and technological advances in glucose monitoring to supportive communities, individuals with diabetes today have access to an array of resources that can significantly improve their quality of life. By fostering awareness and promoting a holistic approach encompassing diet, exercise, emotional well-being, and medical care, individuals living with diabetes can lead full, healthy lives while managing this chronic condition.