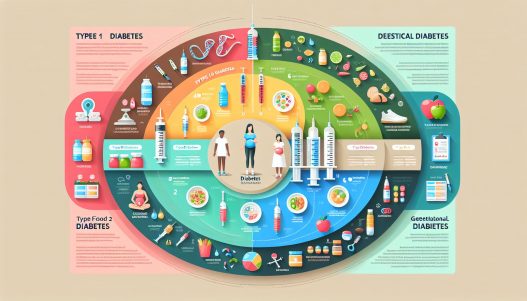
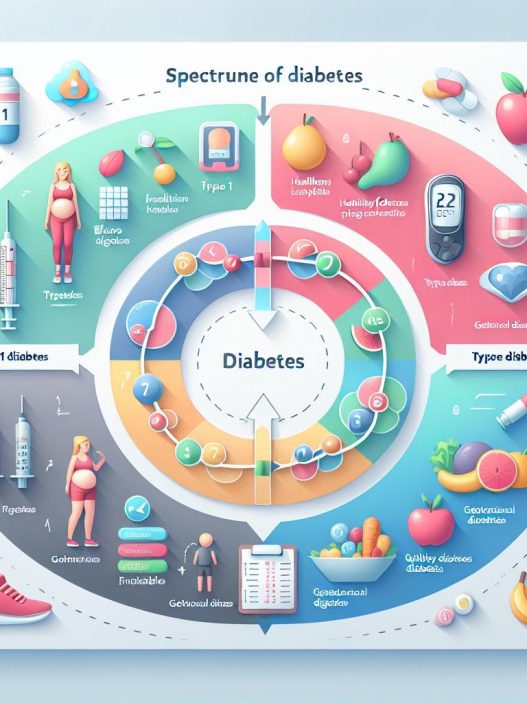
# Understanding the Spectrum of Diabetes: A Comprehensive Guide to Type 1, Type 2, and Gestational Diabetes
Diabetes is a complex condition that impacts millions of lives worldwide, manifesting in various forms, primarily Type 1, Type 2, and gestational diabetes. Each type has its unique pathophysiology, treatment protocols, and implications for individuals affected by them. Understanding these distinctions is crucial for patients, caregivers, and healthcare professionals alike. This comprehensive guide delves into the spectrum of diabetes, illuminating each type’s characteristics, management, and preventive strategies to foster a better understanding of this prevalent condition.
Understanding the Fundamentals of Diabetes: What You Need to Know
Diabetes is a chronic health condition that occurs when the body cannot properly regulate blood sugar (glucose) levels. Glucose is a vital source of energy for our cells, and its regulation is primarily controlled by insulin, a hormone produced by the pancreas. There are two primary mechanisms behind diabetes: insulin resistance and insufficient insulin production. Insulin resistance is most commonly associated with Type 2 diabetes, where the body’s cells fail to respond adequately to insulin. Conversely, Type 1 diabetes is primarily characterized by the pancreas’s inability to produce insulin due to autoimmune destruction of the pancreatic beta cells.
Understanding the prevalence of diabetes is equally important. According to the International Diabetes Federation, around 537 million adults are living with diabetes globally, with projections indicating that this number may rise to 783 million by 2045. This alarming trend highlights the necessity for more awareness, education, and preventive strategies to combat diabetes effectively.
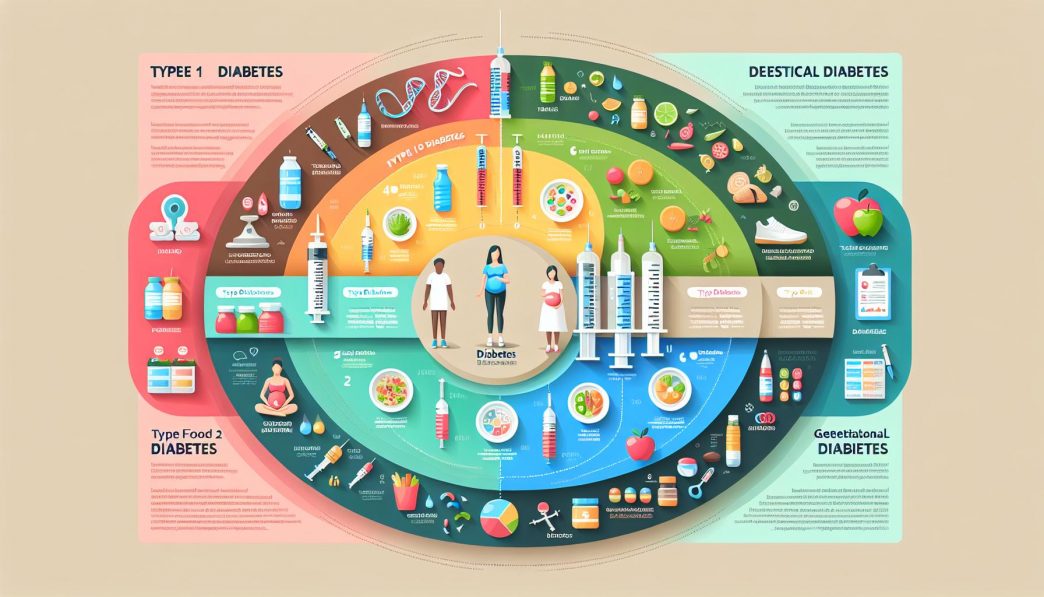
The Distinct Features of Type 1 Diabetes
Type 1 diabetes, formerly known as juvenile diabetes, typically manifests in childhood or adolescence but can occur at any age. This autoimmune condition arises when the immune system erroneously attacks and destroys insulin-producing beta cells in the pancreas. Consequently, individuals with Type 1 diabetes must rely on external insulin administration to regulate their blood sugar levels. Symptoms can develop quite rapidly and may include excessive thirst, frequent urination, extreme fatigue, and blurred vision.
Managing Type 1 diabetes requires a diligent balancing act between insulin administration, diet, and physical activity. People with this type of diabetes often use continuous glucose monitors and insulin pumps to help manage their condition more effectively. Advanced technologies like these have revolutionized diabetes care, allowing for better blood sugar control and improved quality of life.
It’s important to recognize the psychological impacts associated with Type 1 diabetes as well. The constant need to monitor blood glucose levels and manage insulin intake can lead to a phenomenon known as “diabetes burnout.” This term refers to the emotional fatigue experienced by those managing their diabetes. Support from healthcare professionals, family, and peer groups can prove invaluable in combating this psychological toll.
Exploring Type 2 Diabetes: Causes, Symptoms, and Management
Type 2 diabetes is the most prevalent form of diabetes, accounting for approximately 90-95% of all diagnosed cases. Unlike Type 1 diabetes, where the body’s insulin production is drastically reduced, Type 2 diabetes is often characterized by insulin resistance. As the body becomes less effective at utilizing insulin, glucose builds up in the bloodstream, leading to hyperglycemia. Risk factors for developing Type 2 diabetes include obesity, physical inactivity, family history, and age.
Symptoms of Type 2 diabetes can be subtle and may develop slowly over time. They often include increased thirst, excessive hunger, fatigue, and blurred vision. However, many individuals are asymptomatic initially, which is why regular check-ups are crucial for early detection and intervention. In fact, the Centers for Disease Control and Prevention (CDC) recommends annual screenings for high-risk populations.
Management of Type 2 diabetes is multifaceted, involving lifestyle modifications like a balanced diet, regular exercise, and weight management. In many cases, these changes can lead to a significant improvement in insulin sensitivity and blood glucose levels. If lifestyle changes are insufficient, oral medications or insulin therapy might be recommended, which can help individuals achieve better glycemic control. Continuous monitoring of blood glucose levels is also vital, as it allows for timely adjustments in dietary intake, exercise regimens, and medication dosages.
Gestational Diabetes: Understanding Risks and Management
Gestational diabetes occurs during pregnancy and affects approximately 2-10% of expectant mothers. This condition arises when the body cannot produce enough insulin to meet the increased demands of pregnancy. Consequently, blood sugar levels rise, posing risks to both the mother and the developing fetus. Risk factors for gestational diabetes include obesity, advanced maternal age, and a family history of diabetes.
Screening for gestational diabetes typically occurs around the 24th to 28th weeks of pregnancy. If diagnosed, management focuses on maintaining normal blood glucose levels through dietary changes, physical activity, and, in some cases, insulin therapy. Regular monitoring of blood sugar levels is essential to ensure the health of both the mother and child.
While gestational diabetes often resolves after childbirth, it does significantly increase the risk of developing Type 2 diabetes later in life. As such, women who have experienced gestational diabetes should continue to monitor their blood sugar levels and maintain a healthy lifestyle as a preventive measure.
The Interrelationship Between the Three Diabetes Types
Understanding the interplay between Type 1, Type 2, and gestational diabetes is crucial for healthcare providers. Although these conditions originate from different mechanisms, they often share common risk factors and symptoms. For instance, genetics, lifestyle choices, and environmental factors can influence the likelihood of developing any of the three diabetes types.
Education plays a significant role in managing any form of diabetes. Patients and their families should be encouraged to learn about the condition, fostering a sense of autonomy over their health and well-being. This knowledge enables individuals to make informed decisions regarding diet, exercise, and medication, ultimately leading to better management of their diabetes.
Additionally, the role of healthcare professionals cannot be overstated in this context. Regular check-ups, personalized treatment plans, and ongoing patient education are vital components of effective diabetes management. The collaborative approach among patients, healthcare providers, dietitians, and diabetes educators ensures a comprehensive support system for individuals navigating life with diabetes.
Future Trends in Diabetes Management and Prevention
The future of diabetes management looks promising, thanks to ongoing advancements in technology and research. Continuous glucose monitors, insulin pumps, and telemedicine are becoming more accessible and affordable, allowing for improved patient monitoring and real-time support. Additionally, wearable technology is paving the way for innovative ways to manage diabetes on-the-go, such as smartwatches that can track physical activity and sync with glucose monitors.
Moreover, ongoing research into the pathophysiology of diabetes is fostering the development of novel treatments and potential preventive strategies. Anti-obesity medications, GLP-1 receptor agonists, and SGLT2 inhibitors have shown promise in managing Type 2 diabetes, emphasizing the importance of personalized treatment approaches. Ongoing studies into the role of gut microbiota in diabetes management may soon yield groundbreaking insights into prevention and treatment.
Education and awareness campaigns are also vital in combating the diabetes epidemic. Public health initiatives aimed at promoting healthy lifestyles, regular exercise, and balanced diets can significantly impact diabetes prevention. Furthermore, the integration of diabetes management programs in primary healthcare settings promotes early detection and intervention, potentially reducing the burden of diabetes on individuals and healthcare systems.
Conclusion: Empowering Individuals with Knowledge and Support
In conclusion, understanding the spectrum of diabetes—from Type 1 and Type 2 to gestational diabetes—is crucial for patients, caregivers, and healthcare professionals alike. By educating ourselves on the distinct characteristics, management strategies, and ongoing advancements in diabetes care, we can empower individuals to take control of their health and well-being. Prevention, early detection, and comprehensive management are integral components in the fight against diabetes. We must continue to advocate for awareness, understanding, and support for those impacted by this widespread condition, fostering a healthier future for all.
—
This comprehensive guide equips you with detailed insights into the various types of diabetes, their management, and emerging trends in treatment and prevention. By understanding the complexities of this condition, we can promote better health outcomes and pave the way for a brighter future for individuals living with diabetes. Remember, knowledge is power, and with the right tools and support, managing diabetes and leading a fulfilling life is within reach.