# Understanding the Spectrum of Diabetes: A Comprehensive Guide to Type 1, Type 2, and Gestational Diabetes
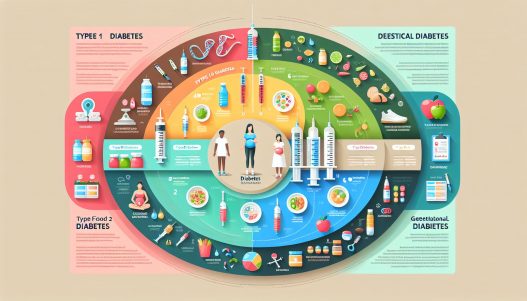
Diabetes mellitus is a chronic condition characterized by high blood glucose levels due to various factors, including insulin resistance and impaired insulin secretion. This comprehensive guide aims to demystify the three main types of diabetes—Type 1, Type 2, and Gestational Diabetes. By understanding the differences, risk factors, symptoms, and management strategies associated with each type, you can take informed steps toward prevention and effective management.
Understanding Diabetes: What You Need to Know
Diabetes is essentially a metabolic disorder that affects how your body utilizes glucose, a primary energy source. In healthy individuals, insulin, a hormone produced by the pancreas, regulates blood sugar levels by facilitating the uptake of glucose into the cells. However, in diabetes, this process becomes dysfunctional, leading to elevated glucose levels in the blood.
Understanding diabetes goes beyond its definition. Several factors contribute to its development, including genetics, lifestyle choices, and environmental influences. By breaking down the complexities of diabetes, we can better equip ourselves to address this global health issue, which affects millions of individuals worldwide.
Type 1 Diabetes: An Autoimmune Condition
What is Type 1 Diabetes?
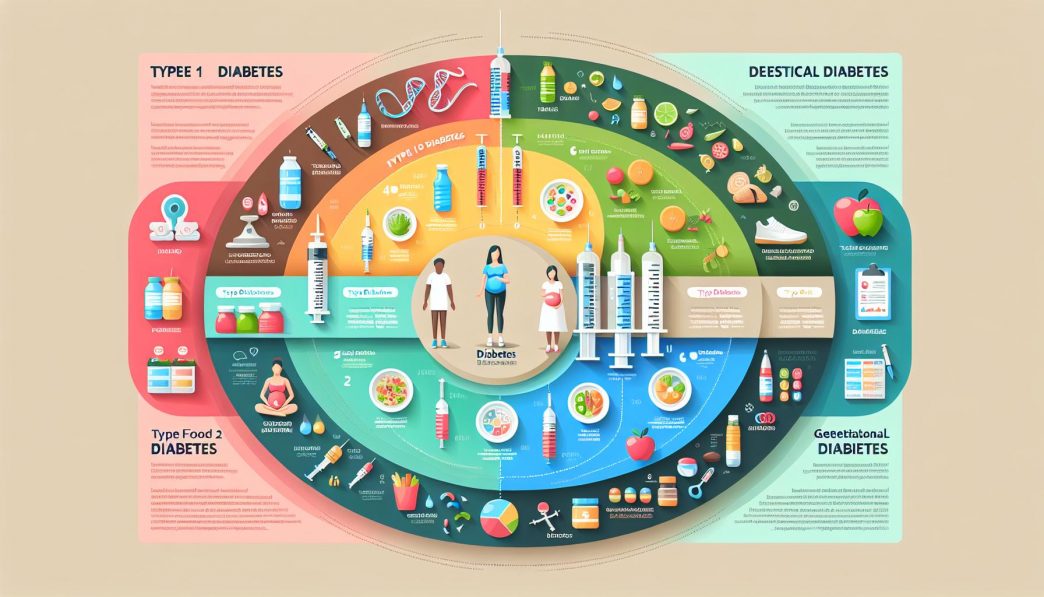
Type 1 diabetes is characterized by the autoimmune destruction of insulin-producing beta cells in the pancreas. This results in little or no insulin production, necessitating lifelong insulin therapy to manage blood glucose levels. Type 1 diabetes typically manifests in childhood or early adulthood, although it can occur at any age.
Individuals with Type 1 diabetes often face unique challenges, including the need for constant blood sugar monitoring, insulin injections or pump therapy, and dietary management. While the exact cause remains unclear, genetics and environmental factors are believed to play significant roles in its onset.
Symptoms and Diagnosis
Common symptoms of Type 1 diabetes include excessive thirst, frequent urination, extreme hunger, weight loss, fatigue, and blurred vision. Since the onset can be rapid, it is crucial to recognize these symptoms early to prevent complications such as diabetic ketoacidosis, a life-threatening condition caused by a shortage of insulin.
Diagnosis typically involves blood tests that measure blood glucose levels. A fasting blood glucose test, oral glucose tolerance test, or A1C test can confirm the presence of diabetes. Early diagnosis and effective management are critical to minimizing the long-term health risks associated with Type 1 diabetes.
Management and Treatment Options
Managing Type 1 diabetes requires a multidisciplinary approach. This includes regular blood glucose monitoring, insulin therapy, and adhering to a balanced diet. Individuals with Type 1 diabetes must also consider how physical activity impacts insulin sensitivity and blood glucose levels.
Education is also vital. Diabetes self-management education (DSME) empowers individuals with the knowledge and skills needed to manage their condition effectively. With advances in diabetes technology, such as continuous glucose monitors (CGMs) and insulin pumps, individuals can achieve better glycemic control and improve their quality of life.
Type 2 Diabetes: A Lifestyle-Related Condition
Understanding Type 2 Diabetes
Type 2 diabetes is the most prevalent form of diabetes, accounting for approximately 90-95% of all diabetes cases. Unlike Type 1 diabetes, it typically develops over time, often as a result of lifestyle factors, including obesity, sedentary behavior, and poor diet. In Type 2 diabetes, the body becomes resistant to insulin, leading to higher blood sugar levels.
Initially, the pancreas compensates by producing more insulin. However, over time, this compensation becomes inadequate, resulting in chronic hyperglycemia. Type 2 diabetes can develop at any age but is more commonly diagnosed in middle-aged and older adults.
Symptoms and Risk Factors
Many individuals with Type 2 diabetes may remain asymptomatic for years, leading to delayed diagnosis. Common symptoms include increased thirst, frequent urination, hunger, fatigue, and blurred vision. Additionally, dark patches of skin, known as acanthosis nigricans, may indicate insulin resistance.
Several risk factors contribute to the development of Type 2 diabetes. These include:
– **Obesity:** Excess body weight, particularly around the abdomen, increases the likelihood of developing insulin resistance.
– **Age:** The risk of Type 2 diabetes increases with age.
– **Family History:** A family history of diabetes can raise an individual’s risk.
– **Sedentary Lifestyle:** Lack of physical activity can lead to weight gain and insulin resistance.
Management and Treatment Strategies
Managing Type 2 diabetes often involves lifestyle modifications such as diet and exercise. A balanced diet rich in whole foods, vegetables, lean proteins, and healthy fats can help control blood sugar levels. Regular physical activity contributes to weight management and improved insulin sensitivity.
In some cases, oral medications or insulin therapy may be necessary to maintain blood glucose levels within normal ranges. Monitoring blood glucose, receiving regular check-ups, and maintaining a healthy lifestyle play vital roles in managing Type 2 diabetes.
Gestational Diabetes: Understanding the Implications
What is Gestational Diabetes?
Gestational diabetes (GD) is a condition characterized by high blood sugar levels that develop during pregnancy. It generally occurs due to hormonal changes that affect insulin action and usually resolves after childbirth. However, gestational diabetes requires careful management to ensure the health of both the mother and baby.
Women typically undergo screening for gestational diabetes between the 24th and 28th weeks of pregnancy. Factors that increase the risk of developing GD include obesity, a family history of diabetes, and certain ethnic backgrounds.
Symptoms and Diagnosis
Gestational diabetes may not present noticeable symptoms, which is why routine screening is essential. When symptoms do occur, they may include increased thirst and hunger, frequent urination, fatigue, and blurred vision.
Diagnosis involves measuring blood sugar levels through an oral glucose tolerance test. If blood glucose levels exceed certain thresholds, a diagnosis of gestational diabetes is made. Early detection and management are essential to minimize complications for both the mother and baby.
Management and Treatment Options
Managing gestational diabetes typically involves dietary changes, regular physical activity, and blood sugar monitoring. Women diagnosed with GD may work closely with healthcare professionals, including nutritionists and endocrinologists, to develop a personalized management plan.
In some cases, insulin therapy may be necessary. It’s crucial for women with gestational diabetes to monitor their glucose levels closely, as uncontrolled blood sugar can lead to complications like macrosomia (large baby), premature birth, and increased risk of cesarean delivery.
The Complications of Diabetes: Understanding the Risks
Long-term Complications of Diabetes
Untreated or poorly managed diabetes can lead to a variety of serious complications. Chronic hyperglycemia affects multiple organ systems, leading to increased morbidity and mortality rates. Some of the long-term complications of diabetes include:
– **Cardiovascular Disease:** Individuals with diabetes are at a higher risk of developing heart conditions, including heart attacks and strokes.
– **Neuropathy:** High blood sugar levels can damage nerves, leading to peripheral neuropathy, characterized by tingling, pain, or loss of sensation in the extremities.
– **Retinopathy:** Diabetes can affect blood vessels in the retina, potentially leading to vision problems and even blindness.
– **Kidney Damage:** Diabetes may lead to nephropathy, resulting in kidney dysfunction or failure.
Psychosocial Implications of Diabetes
Beyond physical health, diabetes can also have psychological impacts. Many individuals with diabetes experience anxiety, depression, or “diabetes burnout,” where the burden of managing the condition becomes overwhelming. Effective diabetes management requires not only physical health support but also emotional and psychological assistance.
Healthcare providers should address these psychosocial factors, as they can significantly affect diabetes management and overall quality of life. Support groups, counseling, and education can play essential roles in helping individuals cope with the emotional challenges of living with diabetes.
Importance of Regular Check-ups and Screenings
Regular health check-ups and screenings are vital for detecting potential complications early. Routine eye exams, foot exams, and kidney function tests can help identify issues before they become severe. Individuals with diabetes should also have regular meetings with their healthcare team to adjust management plans as necessary.
Taking a proactive approach to diabetes management through regular monitoring and health care can prevent complications and sustain a better quality of life.
The Role of Education and Community Support in Diabetes Management
Diabetes Education: Empowering Individuals
Education is a crucial component in managing diabetes effectively. Diabetes self-management education programs teach individuals about nutrition, exercise, blood sugar monitoring, and medication management. These programs empower patients to take control of their diabetes and make informed lifestyle choices.
Support from healthcare providers and diabetes educators can help individuals navigate the complexities of diabetes management. Educational resources can include workshops, informational websites, and support groups that provide valuable information and encouragement.
Community Support: Building a Strong Network
Community support can be instrumental in managing diabetes. Engaging with others who share similar experiences fosters a sense of belonging and provides motivation. Support groups create safe spaces for individuals to share their challenges, successes, and tips for managing diabetes effectively.
Additionally, community programs often offer resources such as exercise classes, nutrition workshops, and wellness events aimed at promoting healthy lifestyles for individuals living with diabetes and their families.
Innovations in Diabetes Care
Advancements in technology and research continue to shape diabetes care, enhancing the lives of those managing this condition. Continuous glucose monitors, insulin pumps, and potential breakthrough medications have transformed diabetes management approaches, providing individuals with more options than ever before.
Research efforts are dedicated to understanding the underlying mechanisms of diabetes and developing new treatment modalities. By staying informed about these developments, individuals can access the most effective tools for managing their diabetes and maintaining a healthy lifestyle.
# Conclusion
Understanding the spectrum of diabetes is essential for effective prevention, management, and support for those affected by this chronic condition. By appreciating the differences between Type 1, Type 2, and gestational diabetes, individuals can make informed decisions about their health. Regular check-ups, a strong support network, and ongoing education empower those living with diabetes to lead fulfilling lives while managing their condition. Through continued research and innovation, the future of diabetes care holds the promise of better management and improved health outcomes for everyone affected by this disease.