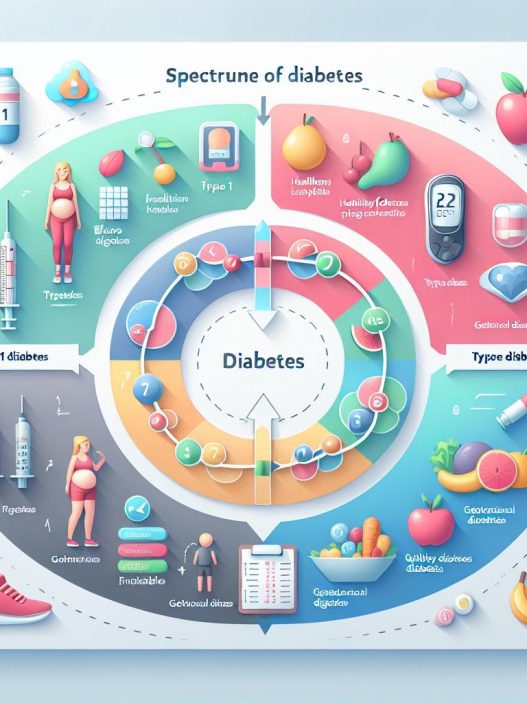
# Understanding the Spectrum of Diabetes: A Deep Dive into Type 1, Type 2, and Gestational Diabetes
Diabetes is a complex and multifaceted disease that affects millions of people worldwide. Understanding the various forms of diabetes, including Type 1, Type 2, and gestational diabetes, is crucial for prevention, diagnosis, and management. This article aims to provide a comprehensive overview of diabetes, examining its causes, symptoms, treatments, and lifestyle implications, empowering readers to take control of their health.
Understanding the Basics of Diabetes
Diabetes is primarily characterized by high blood glucose levels resulting from the body’s inability to produce or effectively use insulin. Insulin is critical for regulating blood sugar, enabling cells to absorb glucose for energy. When this process is disrupted, it can lead to various health complications if not managed effectively. Diabetes is classified into several types, but the three most studied forms are Type 1, Type 2, and gestational diabetes.
The classification into Type 1 and Type 2 is primarily based on the underlying causes and how the body interacts with insulin. Type 1 diabetes typically arises from an autoimmune response that attacks insulin-producing cells in the pancreas. In contrast, Type 2 diabetes is often linked to lifestyle factors, including obesity, poor diet, and physical inactivity. Gestational diabetes occurs during pregnancy and can pose risks to both the mother and child if not adequately managed. Understanding these distinctions can aid in early recognition and appropriate treatment.
Type 1 Diabetes: An Overview
What is Type 1 Diabetes?
Type 1 diabetes is an autoimmune condition where the body’s immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This condition often appears during childhood or adolescence, but it can develop at any age. Individuals with Type 1 diabetes must rely on insulin therapy for life, either through injections or an insulin pump, to manage their blood sugar levels.
Symptoms and Diagnosis
Symptoms of Type 1 diabetes can develop rapidly and may include excessive thirst, frequent urination, extreme fatigue, blurred vision, and unexplained weight loss. These symptoms result from elevated blood sugar levels and the body’s inability to utilize glucose effectively. Diagnosis typically involves blood tests that measure glucose levels and the presence of ketones in the urine, indicating that the body is using fat instead of sugar for energy.
Managing Type 1 Diabetes
Management of Type 1 diabetes involves a combination of insulin therapy, regular blood glucose monitoring, dietary adjustments, and physical activity. Individuals need to learn how to balance their food intake with insulin administration and exercise to maintain healthy blood sugar levels. Continuous glucose monitoring systems are available, providing real-time feedback and making management easier.
Type 2 Diabetes: An In-Depth Look
Defining Type 2 Diabetes
Type 2 diabetes is the most common form of diabetes, usually developing in adults, although it is increasingly seen in children and adolescents due to rising obesity rates. It is characterized by insulin resistance, where the body’s cells fail to respond effectively to insulin, alongside a gradual decline in insulin production. This dual defect results in elevated blood sugar levels over time.
Risk Factors and Symptoms
Several risk factors contribute to the development of Type 2 diabetes, including obesity, sedentary lifestyle, family history, and certain ethnic backgrounds. Common symptoms include increased thirst, frequent urination, fatigue, slow-healing sores, and blurred vision. However, many individuals may remain asymptomatic, making regular screenings essential, particularly for those with risk factors.
Treatment and Lifestyle Modification
Management of Type 2 diabetes often includes lifestyle modifications such as adopting a balanced diet, increasing physical activity, and losing weight. In some cases, medication may be prescribed to help improve insulin sensitivity or reduce glucose production by the liver. Regular monitoring of blood glucose levels is vital for making informed decisions about food, exercise, and medication management.
Gestational Diabetes: Causes and Implications
Understanding Gestational Diabetes
Gestational diabetes occurs during pregnancy, typically around the 24th week, when the body cannot produce enough insulin to meet the increased demands. This condition affects both the mother and the developing fetus, increasing the risk of complications during pregnancy and delivery. Understanding risk factors, symptoms, and management strategies is crucial for ensuring the health of both mother and child.
Risk Factors and Symptoms
Women with a family history of diabetes, those who are overweight, or those who have had gestational diabetes in previous pregnancies are at a higher risk. Symptoms may not always be noticeable, which is why regular screening during pregnancy is essential. Common indicators could include increased thirst and frequent urination, but many women face no obvious symptoms.
Management Strategies for Gestational Diabetes
Managing gestational diabetes typically involves a multidisciplinary approach, including dietary changes, physical activity, and regular monitoring of blood glucose levels. Many women can manage their condition through lifestyle changes, but some may require insulin therapy or oral medications to keep blood sugar levels within a healthy range. Effective management is crucial in minimizing risks for both the mother and the baby.
Common Myths about Diabetes Debunked
Myth 1: Diabetes is Not a Serious Condition
A common misconception is that diabetes is a benign condition that can be easily managed. In reality, uncontrolled diabetes can lead to severe health complications, including heart disease, kidney failure, and vision loss. Awareness of the serious implications of diabetes is vital for proactive management.
Myth 2: Only Overweight People Get Type 2 Diabetes
While obesity is a significant risk factor for Type 2 diabetes, it is not the only one. Individuals of normal weight can also develop Type 2 diabetes, often due to genetic predisposition, sedentary lifestyle, or metabolic factors. Education about all risk factors is essential for prevention and early diagnosis.
Myth 3: People with Diabetes Cannot Eat Sugar
Another prevalent myth is that individuals with diabetes should completely avoid sugar. While monitoring carbohydrate intake is necessary for blood sugar management, it is not about completely eliminating sugar but rather about moderation and making informed food choices. People with diabetes can enjoy sweets in moderation as part of a balanced meal plan.
Conclusion: Empowering Yourself in the Journey with Diabetes
In conclusion, understanding the spectrum of diabetes—Type 1, Type 2, and gestational diabetes—is crucial for effective management and prevention. Education and awareness about the symptoms, risk factors, and treatment options empower individuals to take control of their health. Regular screenings, healthy lifestyle modifications, and ongoing research into diabetes care can significantly improve the quality of life for those living with this condition. By fostering a deeper understanding of diabetes, we can create a supportive community that inspires healthy choices and proactive management strategies.
With ongoing advancements in diabetes research and technology, there is hope for better management options and potential cures in the future. Whether you have diabetes or are at risk, it is essential to stay informed, engaged, and connected to healthy resources.