# Understanding the Spectrum of Diabetes: Exploring Types, Causes, and Management Strategies
Diabetes is a complex and multifaceted health condition affecting millions worldwide. It encompasses a spectrum of disorders characterized by high blood sugar levels due to issues with insulin production, action, or both. Understanding the spectrum of diabetes—ranging from Type 1 to Type 2 diabetes, as well as gestational diabetes and other rarer forms—is essential for effective management. This blog delves into the different types of diabetes, their causes, and strategic management approaches to improve the quality of life for those affected.
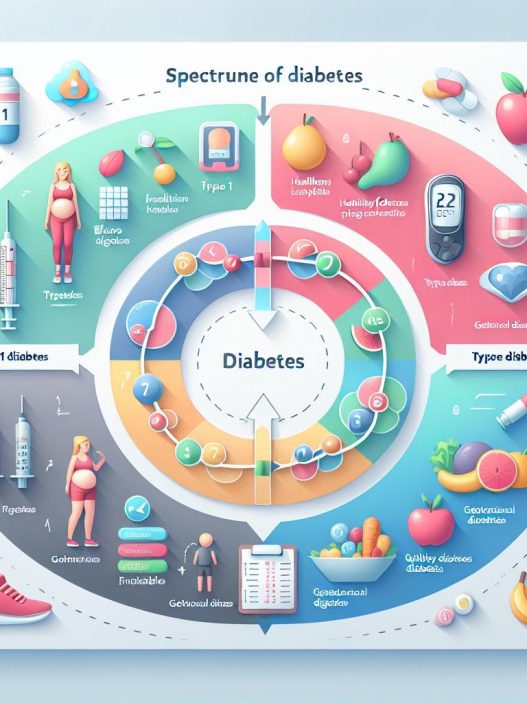
Understanding the Different Types of Diabetes
Diabetes is not a singular disease but rather a classification of disorders with distinct pathophysiological mechanisms. The two predominant forms, Type 1 and Type 2 diabetes, have vastly different causes, symptoms, and management strategies. Type 1 diabetes is primarily an autoimmune condition wherein the body attacks insulin-producing beta cells in the pancreas. This form of diabetes tends to manifest in childhood or early adulthood, although it can occur at any age. The complete insulin deficiency leads to an urgent need for insulin therapy to regulate blood glucose levels effectively.
Type 2 diabetes represents a broader spectrum that often begins with insulin resistance—where the body’s cells do not respond effectively to insulin. Over time, the pancreas is unable to produce enough insulin to compensate, leading to elevated blood sugar levels. Risk factors for Type 2 diabetes include obesity, sedentary lifestyle, and a family history of diabetes. Unlike Type 1, this form of diabetes is more commonly diagnosed in adults but has increasingly been found in younger populations due to escalating obesity rates.
Causes of Diabetes: Debunking the Myths
The causes of diabetes are intricate and can involve a combination of genetic, environmental, and lifestyle factors. In Type 1 diabetes, the autoimmune nature of the disease is still not entirely understood, but it is believed that genetic predisposition, combined with environmental triggers—such as viral infections—plays a crucial role in its onset. This can lead to the destruction of insulin-producing cells and ultimately insulin deficiency.
On the other hand, Type 2 diabetes often results from a combination of lifestyle factors that contribute to insulin resistance. Conditions such as obesity, inactivity, a diet high in refined carbohydrates and sugars can exacerbate the condition. Persistent high blood sugar levels can further lead to increased fat accumulation around the abdomen, creating a vicious cycle. Genetic factors also contribute significantly, as individuals with a family history of Type 2 diabetes possess a higher risk of developing the disease themselves.
Exploring the Symptoms of Diabetes
Recognizing the symptoms of diabetes can be vital for early diagnosis and management. Common symptoms of both Type 1 and Type 2 diabetes include increased thirst, frequent urination, extreme fatigue, and blurred vision. In Type 1 diabetes, symptoms often develop rapidly and may be accompanied by unexplained weight loss, as the body starts to draw energy from fat and muscle stores in the absence of insulin. Ketoacidosis, a severe complication of Type 1 diabetes, can lead to nausea, vomiting, abdominal pain, and confusion, necessitating immediate medical intervention.
Type 2 diabetes symptoms may develop gradually, and many individuals may remain asymptomatic for years until complications occur. These complications can include nerve damage, kidney problems, cardiovascular issues, and vision loss, leading to a higher risk of heart disease and stroke. Therefore, regular screening and monitoring are crucial for those at risk, particularly with lifestyle factors contributing to the onset of Type 2 diabetes.
Risk Factors for Diabetes: Who Is at Risk?
Certain risk factors significantly increase the likelihood of developing various types of diabetes. For Type 1 diabetes, while anyone can develop it, it is more common in individuals under 30, and those with a family history of the disease or autoimmune conditions are at increased risk. Infectious agents and environmental toxins may also contribute, although these relationships remain unclear.
Type 2 diabetes, however, showcases more identifiable risk factors. Age is a major contributor, with risk increasing after age 45. Other critical factors include obesity, a sedentary lifestyle, high blood pressure, high cholesterol, and a family history of diabetes. Moreover, specific ethnic groups—such as African Americans, Hispanic Americans, and Native Americans—experience higher rates of Type 2 diabetes. Identifying these risk factors in individuals can guide preventive strategies and interventions to mitigate the onset of the disease.
Management Strategies for Diabetes: A Holistic Approach
Management of diabetes is a multifaceted endeavor aimed at controlling blood sugar levels and mitigating complications through various lifestyle modifications and medical interventions. For individuals with Type 1 diabetes, insulin therapy is a cornerstone of management, often supplemented with ongoing blood glucose monitoring and a balanced diet to maintain healthy sugar levels. Continuous glucose monitors (CGMs) have dramatically transformed management strategies by allowing patients to track glucose levels in real time, making necessary adjustments more manageable.
Type 2 diabetes management focuses largely on lifestyle changes, including weight loss, increased physical activity, and dietary modifications. The Mediterranean diet and plant-based diets have shown great promise in managing blood sugar levels effectively. Medications may be introduced when lifestyle changes alone do not achieve adequate glucose control. This includes the use of oral hypoglycemics, glucagon-like peptide-1 (GLP-1) receptor agonists, and insulin therapy for more advanced cases.
Moreover, a comprehensive approach to diabetes management also stresses the importance of regular physician appointments, routine laboratory tests for monitoring glycosylated hemoglobin (A1C), and screenings for complications associated with diabetes such as retinopathy and neuropathy. Support systems, including diabetic education and community engagement, play crucial roles in sustaining effective management strategies.
—
This content provides a comprehensive overview of diabetes, diving deep into its spectrum, causes, symptoms, risk factors, and management strategies. A thorough understanding helps demystify this chronic condition while empowering individuals to take control of their health.