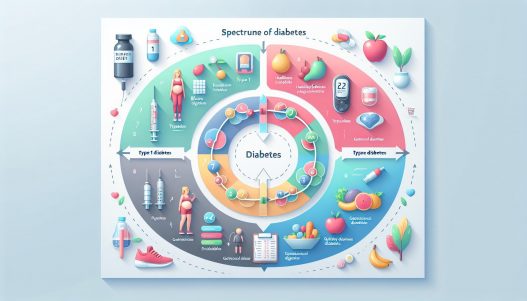
# Understanding the Spectrum of Diabetes: From Type 1 to Type 2 and Beyond
Diabetes is a chronic medical condition that affects how the body processes glucose, the primary source of energy for our cells. It can range from minimal insulin resistance to total insulin deficiency, leading to a spectrum of diabetes types, most notably Type 1 and Type 2 diabetes, as well as an array of other less common forms. Understanding the nuances of these categories is crucial for prevention, management, and improving the quality of life for those affected.
Understanding Type 1 Diabetes: Causes and Management
Type 1 diabetes is primarily an autoimmune condition where the body’s immune system mistakenly attacks and destroys insulin-producing beta cells in the pancreas. This results in little to no production of insulin, a hormone critical for regulating blood sugar levels. The exact cause of Type 1 diabetes remains a mystery, but genetic predisposition combined with environmental factors such as viral infections is believed to play a role.
Management of Type 1 diabetes revolves around maintaining optimal blood sugar levels through insulin therapy, which can be administered via injections or an insulin pump. Additionally, continuous glucose monitoring (CGM) systems help individuals track their blood glucose levels in real-time, allowing for timely interventions. A balanced diet, regular physical activity, and education about diabetes management are key components that empower individuals to lead healthy lives despite their condition.
The Rise of Type 2 Diabetes: Contributing Factors and Prevention
Type 2 diabetes, comprising around 90-95% of all diabetes cases, often develops due to insulin resistance, where the body’s cells become less responsive to insulin. It is closely linked to lifestyle factors, particularly obesity, physical inactivity, and poor dietary habits. Genetics also plays a crucial role, making some individuals more susceptible than others.
Preventing Type 2 diabetes involves lifestyle modifications including weight management, regular physical activity, and a healthy, balanced diet rich in whole grains, fruits, vegetables, and lean proteins. The role of regular health screenings cannot be overstated, as early detection of prediabetes can lead to interventions that may reverse or delay the onset of the disease. Programs involving education on nutrition, exercise, and stress management can be instrumental in reducing one’s risk.
Gestational Diabetes: Understanding the Temporary Condition
Gestational diabetes occurs during pregnancy when hormonal changes cause insulin resistance, leading to elevated blood glucose levels. Although this condition typically resolves after childbirth, both the mother and child may experience health complications during and after the pregnancy. Risk factors include obesity, a family history of diabetes, and advanced maternal age.
Management of gestational diabetes focuses on blood sugar control through dietary adjustments, exercise, and, if necessary, insulin therapy. Regular monitoring of blood glucose levels is essential to ensure the safety of both the mother and the developing fetus. After delivery, women who have had gestational diabetes should continue monitoring their blood sugar since they are at a higher risk of developing Type 2 diabetes later in life.
Other Specific Types of Diabetes: An Overview
While Type 1 and Type 2 comprise the majority of diabetes cases, several other specific types also warrant attention. These can include LADA (Latent Autoimmune Diabetes in Adults), MODY (Maturity Onset Diabetes of the Young), and secondary diabetes caused by other diseases or medications. Each type presents its own set of challenges and management guidelines.
LADA shares characteristics with both Type 1 and Type 2 diabetes, often developing in adults over the age of 30. It can lead to insulin dependency over time, despite initially being treated with lifestyle changes or oral drugs. MODY, on the other hand, is a rare genetic form of diabetes that usually manifests in adolescence or early adulthood and can often be managed without insulin. Secondary diabetes occurs as a result of other medical conditions such as pancreatitis or from the use of certain medications, requiring tailored management strategies to address the underlying cause.
Living with Diabetes: Psychological and Social Implications
Diabetes is not just a physical health issue; it can take a significant psychological toll on individuals. From the routine finger sticks to the constant blood sugar monitoring, the daily management of diabetes can be overwhelming and stressful. Anxiety, depression, and diabetes distress—feelings of frustration or burnout related to diabetes self-management—are common among those living with diabetes.
Social support plays a critical role in managing these psychological challenges. Engaging with healthcare providers, joining support groups, or involving family and friends can alleviate feelings of isolation and provide much-needed encouragement. Educational resources, counseling, and mental health services are also vital in helping individuals navigate the emotional landscape associated with diabetes.
The Future of Diabetes Care: Innovations and Research Directions
The landscape of diabetes care is rapidly evolving, with innovations in technology and research paving the way for better management strategies. Continuous advancements in insulin delivery systems, like closed-loop systems that automate insulin delivery based on glucose levels, are revolutionizing insulin therapy for individuals with diabetes. Furthermore, the exploration of advanced diabetes drugs and therapies aims to improve glycemic control, reduce the risk of complications, and enhance overall quality of life.
Research is also increasingly focusing on the prevention of diabetes, especially in at-risk populations. Efforts to better understand the molecular and genetic foundations of diabetes can lead to revolutionary prevention strategies and potential cures. Awareness of diabetes’ multifaceted nature—covering lifestyle, genetics, and psychology—highlights the need for comprehensive care that integrates medical, nutritional, and psychological support.
In conclusion, understanding the spectrum of diabetes from Type 1 and Type 2 to gestational and other specific types is vital for effective management and care. With ongoing research, embracing technological advancements, and addressing psychological impacts, we can foster an environment that promotes healthier living for individuals affected by diabetes, ultimately aiming for improved outcomes and quality of life. Through education, awareness, and continuous support, it is possible to navigate the complexities of diabetes and build a brighter future for those living with this condition.